It is a refrain that Erbin-Roesemann hears frequently now from her students and their families as the director of the St. David’s Texas State University School of Nursing program in Round Rock. And in Texas in recent years, the adage is still true.
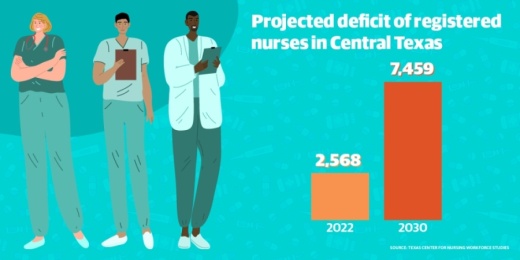
According to data from the Texas Center for Nursing Workforce Studies, Central Texas is projected to face a shortage of 2,568 registered nurses by 2022, and in 2030 that deficit is projected to go up to 7,459 full-time equivalent positions. Statewide, according to the report, the gap between the number of registered nurses needed and the number working in 2030 is projected to be nearly 60,000.
This is not a new problem for Central Texas, where population growth has fueled a corresponding increase in medical needs. Adding to that demand is the short career span for the high-stress position of a registered nurse working at the beside of patients in the hospital. Erbin-Roesemann said nursing managers have told her they are lucky to keep a nurse for two years before that employee moves on to another role.
And Central Texas is aging, not just in its population—10.2% of the metro area is age 65 or older—but among nurses as well.
“The majority of our workforce now is baby boomers. They are of retirement age; that’s what’s causing us to see this shortage increase again,” said Serena Bumpus, the practice director of the Texas Nurses Association.
As cases of the coronavirus continue to rise locally, the consequences of that longstanding shortage could be significant for the community.
Not enough beds, not enough nurses
As of March 30, there have been 206 confirmed cases of the coronavirus in Travis County and 50 in Williamson County, including three total deaths. Local hospital resources have not yet been strained, but Dr. Mark Escott, the interim health authority for Austin Public Health, said March 26 that if local residents do not cut down ten-fold on their normal daily interactions through social distancing, the area could face a shortage of 20,000 hospital beds by June.
Anne Blumofe is a nurse who cares for patients on a medical-surgical floor at a local hospital. She said her team has been preparing for what may be coming and getting briefed daily on the evolving recommendations for best practices.
“I think there’s a lot of sadness and suspense; I think that I speak for most of the people that I work with when I say that we want to take care of people. We want to do our part,” Blumofe said. “The good thing is that each day that goes by before we have a massive influx gives us a chance to hopefully be better prepared to protect ourselves and our families.”
University of Texas models show that even with a 75% reduction in daily contacts among residents, hospitalizations may exceed the capacity of local facilities this summer.
“I think Travis County, Williamson County, we’re all preparing for what happens when we run out of beds, and we’re all praying that we don’t,” Erbin-Roesemann said.
Bumpus said normally nurses would have a 1-2 ratio with patients in critical care, meaning one nurse could care for two patients. However, if patients are intubated—or breathing through a plastic tube to receive adequate oxygen—that ratio drops to 1-1.
“We haven’t looked far enough ahead to see, ‘How many nurses does this mean we need to take care of these patients?’ Our local hospitals have, but in workforce planning at the state level, I don’t know if we know what that looks like,” Bumpus said.
Educational resources
On March 21, Gov. Greg Abbott waived certain Texas Board of Nursing regulations that could allow more nurses to to assist in the state’s coronavirus recovery efforts.
One of those waivers allowed graduates from a nursing program to extend their temporary permits to practice for up to six months, rather than the original 75-day length of the permit, before taking their licensure exams.
That means the 101 seniors in Erbin-Roesemann’s program can apply for their license in May after graduation and devote all of their immediate focus on their work with patients.
“They’re ready to graduate. Maybe more so this year, they see the need and want to be out there,” Erbin-Roesemann said.
Previously, those soon-to-be nursing graduates could only complete half their clinical coursework in a simulated environment, but with many universities closing their campuses, the requirements were waived to allow students to finish their studies under safe conditions and graduate on time.
In August, Austin Community College graduated its first class in its program that allows licensed registered nurses to receive a Bachelor of Science in Nursing, also known as RN to BSN. It helps health care organizations that want a more educated workforce, and it helps the students by opening up more career opportunities. Blumofe was a member of that first class over the summer, and while she was not working during the program, many of her peers were.
On April 2, ACC faculty member John Nation will begin his first class of the spring semester with his RN-to-BSN students, many of whom are studying to receive their bachelor’s degrees even as they are at the forefront of the community’s effort to overcome the coronavirus.
“They’re already registered nurses and are fulfilling critical roles in our community. It’s a unique time; I don’t think it’s anything like any nurse educator has ever seen before,” Nation said. “We’re focusing on supporting our students and doing the best job we can.”
Nurses answer the call
Data from Workforce Solutions of the Capital Area shows that between 2016-26, the number of available registered nurse positions in Central Texas is projected to grow to 3,225, along with 236 openings for nurse practitioners, 527 licensed vocational nurses and 904 certified nursing assistants.
Those gaps cannot be filled immediately with new graduates from nursing school or licensed nurses receiving additional education to further their careers, so hospitals are doing all they can to fill the gaps with the staff they have.
According to Bumpus, Abbott’s recent decision to postpone elective surgeries allowed nurses who have a critical care background to be redeployed in emergency rooms or intensive care units in order to meet the projected need of the community.
“It’s another set of hands and resource our hospitals are tapping into,” Bumpus said.
Nurses who are retired or let their licenses expire will also be able to re-enter the workforce more easily thanks to another waiver Abbott approved March 21 that exempts certain requirements and fees.
Bumpus said the nurses she has talked to who have asked about reactivating their licenses have expressed a desire to help their fellow nurses in the profession any way they can.
“There’s this innate need we have as nurses to step up. For a nurse who is retired who has put in more than their fair share of time, for them to come back in and help in some way, it’s admirable, it makes you proud to be a nurse,” she said.
Meanwhile, nurses, medical professionals and community members are breathing a small sigh of relief with every day that goes by without a significant spike in hospitalizations locally. Blumofe said when she went back to school and began working as a nurse, she could not have predicted this—but she is ready to be part of the solution.
“None of us know when it might be our own loved ones who need care. When you’re able to provide that to someone else, you feel a little less powerless in the face of something unknown,” she said.