Kelsea Heiman, an emergency room nurse at Houston Methodist Clear Lake Hospital, said nurses have felt a lot of extra weight on their shoulders while treating patients as COVID-19 guidelines continue to evolve. This has led to a sense of exhaustion for the nurses putting aside their own fears to provide patient care, she said.
“COVID[-19] has caused a lot of burnout,” she said. “People are starting to evaluate [their] work-life balance.”
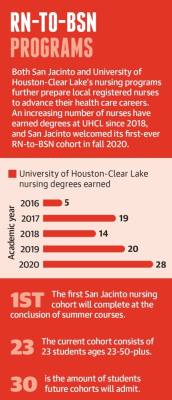
Educators at the University of Houston-Clear Lake and San Jacinto College also described a change in classrooms during the pandemic as both schools trained registered nurses in their RN-to-BSN programs. Working RNs can earn a bachelor’s degree in nursing at both universities, so UHCL and San Jac students have been coping with the realities of COVID-19 in the field while doing coursework.
These realities have led to the exacerbation of an already-present nursing shortage across the Texas Gulf Coast region, which includes Houston, local and regional experts said.
The Texas Department of State Health Services projects the Gulf Coast will have a deficit of 21,400 registered nurses by 2032 as the growing demand continues to outweigh the supply. Though the region’s supply of registered nurses has grown 45% in the last decade, according to the DSHS, experts said that growth is not enough to keep up with the population.
“The nursing workforce is just being stretched, and with that you lose quality,” Heiman said, describing the consequences of an overworked nurse caring for many critically ill patients and simultaneously keeping families informed of their conditions. “Who wants to be cared for by a bitter, cranky nurse?” Changing educational landscapes
Local educators are refining their programs to account for the changing needs of today’s patients, nurses and nursing faculty.
The first-ever cohort of BSN students started at San Jacinto in fall 2020 and will graduate at the end of the summer 2021 session. These students were applying for and completing the program during a pandemic, which necessitated making time in the classroom to properly address the effects of COVID-19 on students’ and staff’s lives, said Rhonda Bell, San Jacinto’s dean of health and natural sciences.
Some faculty decided to retire earlier, leaving the remaining instructors susceptible to increased burnout, Bell said. Although she hopes resuming in-person education will re-energize faculty and remind them why they chose education over practice, she expects nursing faculty shortages to be magnified by COVID-19-related fatigue.
“I think we’re going to have some faculty that will end up leaving the education world,” she said.
UHCL’s RN-to-BSN program has awarded nearly 90 nursing bachelor’s degrees in the last five academic years, per university data. Program classes are all taught at the Pearland campus, university officials said; UHCL opened a three-story, $24.6 million facility in 2019 to allow for expansion of its health care degree programs.
RN-to-BSN program director Karen Alexander echoed Bell’s sentiment that the effects of COVID-19 are felt by nursing instructors.
“We, too, are going through something, living the experience through the eyes of the students,” she said.
Alexander teaches her students to accept, adapt and overcome while working as nurses and facing adversity. Many students have had field work opportunities vanish or become otherwise complicated due to COVID-19 regulations, she said.
These students are experiencing complications around finishing their coursework while already being under pressure from the competitiveness of their programs. The DSHS reported 54% of qualified applicants were not granted admission to one of the region’s 27 prelicensure registered nurse education programs in 2019 due to a limited number of seats available. Still, watching nurses work through a public health crisis seems to have motivated the next generation to seek a career in health care, Bell said.
“I think that they have been inspired, watching what nurses have been doing for this past year and a half,” she said. “It has inspired them to stay focused and get this BSN because they see the potential growth in their careers as they do that.”
Addressing pay equity
Remedying the nursing shortage involves caring for the social and emotional needs of current students but also involves furthering nurses’ education past a BSN and providing for better educator pay, experts said.
The nursing faculty turnover rate for Gulf Coast-area programs in 2019 was approximately 13%, and the faculty vacancy rate was 6.5%. Faculty pay equity remains an issue when it comes to addressing the shortage, said Dr. Renae Schumann, the former dean of Houston Baptist University’s School of Nursing and Allied Health who now serves as District 9 president of the Texas Nurses Association.
“We absolutely need more faculty, which means that the schools have to pay the faculty something that they consider desirable enough to leave the hospital,” she said. Nurses experiencing burnout may choose to take their career in another direction by going into nursing administration, Alexander said. UHCL’s course offerings focus specifically on leadership and management, aiming to help working nurses sharpen their skills and prepare for this career shift.
Alexander said 98% of UHCL’s program graduates go on to complete graduate and doctoral degrees, which are necessary qualifications to be a nursing educator. However, investing time, money and effort into nursing school at any level is grueling, said Heiman, who has been a nurse for seven years.
“Life is expensive,” Heiman said. “The money is just not there.”
Nurses with doctoral degrees working in administration or leadership positions can earn significantly more than a nursing educator makes, Alexander said, which makes rectifying the shortage of educators an uphill battle.
“You need to find those who are dedicated to [nursing education] because they love it, not because of the money,” Alexander said.
Nursing administrators in Houston can make, on average, $20,000 more per year than their nursing faculty colleagues, according to data from ZipRecruiter and Payscale.com. The average annual pay for a Houston nursing administrator is about $89,000, while nursing faculty make an average of about $68,000 annually.
Aging populations and telehealth
For the local nurses choosing to enter or remain in the field, they are caring for more senior patients while dealing with an aging workforce and grappling with how to employ telehealth.
About 1 in 4 Gulf Coast nurses is over age 55. These nurses are treating an aging population: About 10.5% of Houston and League City residents are age 65 and older, according to 2019 U.S. census data, up from the about 9.5% of residents over 65 in these cities who were identified in 2014 census data.
As telehealth increases in prevalence, screens and remote options present new challenges for nurses, nursing educators and patients. Students need to learn how to handle scenarios unique to telehealth as it increases in prevalence, meaning educators must be responsive to how the technology could change standards and practices, Bell said.
Telecommunications can make the process of treating older patients more difficult, Heiman said, as the patients attempt to navigate the new technology and advocate for themselves at the same time. The use of telehealth involves patients having consistent access to the technology needed for remote medical care, which is also not always possible, Heiman said.
The logistical difficulties leave nurses wondering if anything was lost in translation or otherwise unwittingly glossed over, she said.
“I think telehealth is going to change things a lot, and I don’t know if it’s for the better,” Heiman said. The median turnover rate in 2019 for registered nurses in the Gulf Coast region was 17.5% in hospitals but much higher in long-term care facilities at 50%. COVID-19 made in-person patient care difficult for the staff at skilled nursing center Focused Care at Webster, Executive Director of Operations Kristin Turner said.
Quarantine policies often meant redistributing tasks among remaining staff while trying to minimize the number of people working in multiple buildings to minimize exposure, she said. The addition of more personal protective equipment also compromises or limits nurses’ interactions with residents, Turner added.
Nurses have had to adapt their care practices to keep residents happy and healthy while also navigating new, changing standards for family visitations and excursions. Facility leaders encourage staff to address their burnout if needed and to remember why they chose this particular branch of nursing, Turner said.
“It has been a long, treacherous year, and everybody is tired,” she said.
Haley Morrison and Danica Lloyd contributed to this report.