Galveston County released the combined total of confirmed cases for both area facilities, as it did with outbreaks in two Texas City nursing homes, making it impossible to tell how many cases there were where Fremont’s grandmother lives. Relatives repeatedly attempted to obtain specifics, Fremont said, but were eventually told by a social worker that county health department regulations prohibit releasing more information to families. Health department officials did not respond to a request for further comment on the data.
There is a feeling of unease, with relatives unable to visit loved ones or find out exactly how at risk they are, Fremont said.
“We have a very vulnerable set of population that is locked away; nobody can really check on them, and the people that have the ability to check on them are not being forthcoming,” she said.
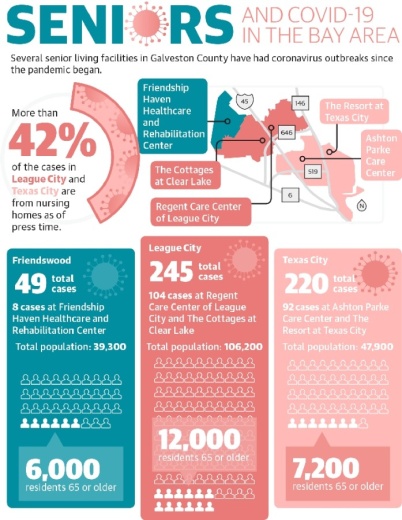
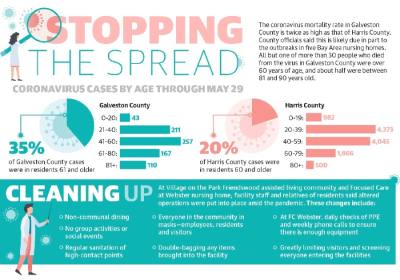
Galveston County’s coronavirus mortality rate is about 4.2%, twice as high as the 2.1% rate in Harris County. All but one of the 32 people who died from the virus in Galveston County were over 60 years of age; roughly half were between 81 and 90 years old.
Staff at local nursing homes, post-acute care centers and senior living communities said the pandemic’s effect on the elderly has been far-reaching, and although they have adapted to manage the spread of the coronavirus, changes are expected to continue as providers navigate post-pandemic senior care.
Response to nursing home outbreaks
In early April, Galveston County reported about 90 residents were infected at The Resort at Texas City and Ashton Parke Care Center in Texas City, accounting for just under half of the city’s 202 total cases. Another 104 cases were reported in League City as of May 29, all from The Cottages at Clear Lake and Regent Care Center of League City, making up more than 42% of the total 245 cases in the city.
The outbreaks are likely part of the reason why Galveston County’s COVID-19 mortality rate is twice as high as Houston’s and Harris County’s, Zach Davidson, communications director for Galveston County Judge Mark Henry, told Community Impact Newspaper.
Staff at The Resort at Texas City, Ashton Parke Care Center, The Cottages at Clear Lake and Regent Care Center of League City did not respond to multiple requests for comment on the outbreaks. As of May 20, case counts at the League City facilities were increasing.
Derek Prince, CEO of the parent company of Friendship Haven Healthcare and Rehabilitation Center in Friendswood where eight cases were confirmed, said the facility began testing all residents, patients and employees for coronavirus a week ahead of Gov. Greg Abbott’s order to do so.
“Our nursing facilities, with communal settings and frail population, present a delicate setting for care and treating this novel virus,” Prince said in a statement. “Testing everyone in our facility allows us to properly isolate and quarantine our residents and employees. We are notifying all family members about this testing and results and working with our state and local officials.”
Friendship Haven did not respond to requests for further comment.
Abbott announced May 11 that 100% of Texas’ nursing home residents and staff members will be tested for coronavirus, but did not provide a timeline for when testing would begin. The state’s Health and Human Services Commission, Division of Emergency Management and Department of State Health Services received direction from Abbott to implement a plan based on guidance from Vice President Mike Pence and Coronavirus Response Coordinator Dr. Deborah Birx. Testing is only mandated for skilled nursing facilities, not assisted living communities, Harris County Public Health officials said May 20.
Focused Care at Webster had six residents with confirmed cases, all asymptomatic, said Mark McKenzie, CEO of Focused Post Acute Care Partners. Four employees also tested positive but have since returned to work after later testing negative, as required, he said.
No deaths have been reported at the facility, and it is coronavirus-free as of May 18, McKenzie said. In late March, the facility started to monitor shared employees—those who work in multiple facilities—in all Focused Care communities and made the decision in early April to prohibit shared employees from working in the facilities, he added.
The facility will continue to be proactive and exceed national health guidance when necessary to care for residents, McKenzie said.
“Focused Care, in some cases, exceeded recommendations and guidance from the Centers for Disease and Prevention Control since the onset of the spread of the pandemic,” he said in an email. “Our preparation and continued diligence are a reflection of our mission to care for residents prior to the pandemic and will continue as we all adjust to a post-pandemic world.”
Post-pandemic changes for seniors
Local facility managers said the environments at nursing homes, post-acute care centers and senior living communities will be distinctly different after the coronavirus pandemic.
Skilled nursing providers across the country are learning many of the pandemic’s unintended consequences and, in turn, some of the flaws in the health care system, McKenzie said. The long-term care workforce is historically underpaid, leading to high turnover, he said. A national study released April 23 by the Kaiser Family Foundation indicates long-term care employees are disproportionately lower-wage workers.
Texas’s rate of Medicaid funding does not cover the actual cost of care for residents, McKenzie added, and he called on lawmakers to reconsider this rate moving forward.
“Health care providers, patients, consumers and policymakers must take into consideration where we were before the pandemic crashed on our shores and where we should be in the future,” he wrote.
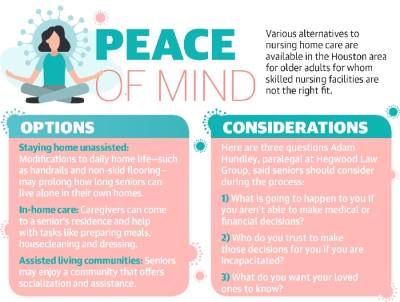
Mark Fritz, president of Bridgemoor Transitional Care in Webster, agreed the pandemic provided facilities with learning opportunities. After major medical procedures, some seniors may spend time at a post-acute center such as Bridgemoor, which provides short-term rehabilitative care like an extension of a hospital, Fritz said. The goal at a place such as Bridgemoor is to get patients back home quickly and safely, since home is the safest place for elderly people, he added.
As a result of the pandemic, patients and their relatives will likely be more selective when choosing a care center, he said.
“I think people are going to look very differently at what type of post-acute care they’re going to,” Fritz said.
Jeffery Smith, senior vice president of sales and marketing for The Shores at Clear Lake, said the last several months have underscored the necessity of isolation for residents at the assisted living facility. At The Shores at Clear Lake, residents will likely continue sheltering in place as the state reopens, and the community’s no-visitors rule is expected to continue, Smith said.
“Our world—kind of living in a bubble with our residents and our communities—that’s not going to change for a while,” he said. “It’s going to be this protective bubble still, until a vaccine comes out.”
The staff continues to adapt its touring and move-in process, as seniors’ needs for housing and care have not been put on hold, Smith said. The community “recently had a confirmed case of COVID-19 that has since been cleared in accordance with CDC guidelines,” according to its website. Smith said prohibiting visitors has been a tremendous help in keeping the coronavirus out of the community.
Future elder care considerations
Senior care providers must take into account both the physical and emotional health risks present among elderly populations to properly administer care post-pandemic, according to a community health expert at the University of Houston-Clear Lake.
Part of what makes seniors so vulnerable to the coronavirus is the comorbidities—or co-occurring disorders—many have that put them higher at risk of infection, said Julianna Dean, who teaches in the Department of Clinical, Health, and Applied Sciences at UHCL. These comorbidities include conditions such as asthma and chronic obstructive pulmonary disease.
Moreover, if an elderly person is hard of hearing, more effort may be required to produce speech, which could greatly increase the potential for saliva droplet contamination, she added. Another common source of infection is high-traffic areas such as light switches or, in a nursing facility, handrails and walkers.
Beyond the physical risk factors, older individuals in general experience more loneliness, which over time can be detrimental, Dean said. Not only could the lack of physical touch or quality time with loved ones lead to anxiety and depression, it could also increase seniors’ mortality rate.
“We know that we have to have human contacts—hugs or just time spent with others—and because that is being limited right now, there may be an increase in mortality,” Dean said. “Social interaction is so important for the elderly, and so ways to incorporate that ... can really improve their health.”
The pandemic has greatly compromised the social infrastructure, which Dean referred to as “social capital,” present at many skilled nursing facilities. In many facilities, this social capital takes the form of outings and group activities, which have been virtually eliminated amid the pandemic. Reinstating some form of social infrastructure will be just as essential as providing care for physical ailments in the coming months, she said.
“When we don’t have those good social relationships, our health is compromised regardless of if we go to the best doctors,” she said. “If we don’t have good social capital, regardless of the high standards of care we have, our health could still be bad.”