However, when compared to the state’s estimated 2019 population of nearly 29 million, these vaccination rates lag behind. According to data from the United States Census Bureau, whites represent 41% of the state population, with Hispanics at 39.7%, and Black and Asian populations at 12.9% and 5.2%, respectively.
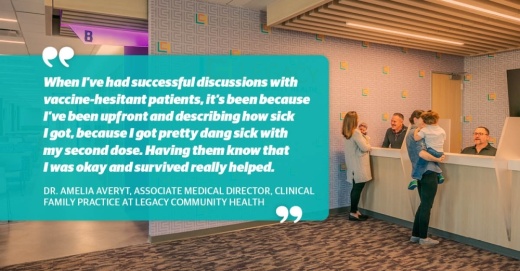
Community Impact Newspaper spoke with Dr. Amelia Averyt, associate medical director of clinical family practice at Legacy Community Health, on the conversations she and other doctors are having with patients who may be hesitant to take a vaccine.
The conversation has been edited for length and clarity.
What is the current situation regarding inoculations in the clinic?
In my clinic there is a mix. We’ve had trouble filling our vaccine clinic openings. When I’m asking patients directly about it, a lot of them have already been vaccinated. Granted, that’s a select pool if they’re coming to the doctor and getting routine health care.
Others are hesitant. A lot of the concerns I’m hearing, whether it’s from patients or patient families, is about the safety of the vaccines. I don’t think the news about the [Johnson & Johnson] vaccine helped that situation much. People were a little bit concerned with how quickly they were developed and rolled out.
People are also scared of the side effects, especially with information they receive shared via social media, as it tends to be very anecdotal. I’ve also heard concerns about fertility, menstruation, and all sorts of things. And then concerns of feeling sick after the vaccine.
I’ve also had nonchalant patients who say, “If I’m going to get it, I’m going to get it. Everybody is going to get it.” They are more resigned to the fact that this got out of our hands and “why should we think that we can control it?”
How do you tackle those challenges?
It’s tough to create messaging that addresses all of those things. One of the approaches I’ve found most effective is through family members having discussions among themselves or reaching out to loved ones or neighbors. So it’s important to empower patients to have the right information on hand and go through that conversation with them so that they can have a discussion with their loved ones.
When I’ve had successful discussions with vaccine-hesitant patients, it’s been because I’ve been upfront and describing how sick I got, because I got pretty dang sick with my second dose. Having them know that I was okay and survived really helped. It also helps to remind them about the new [Centers for Disease Control] guidelines, that there’s more of a benefit to getting vaccinated and taking steps to getting back to normal activities.
How do you start to address underserved communities that might not have as much access to a nearby clinic?
We have an ongoing dedication to getting vaccines into pockets of Houston that otherwise may not see the vaccine. We’ve also got a lot of community partnerships through local government and national government as well.
In Houston, on the east side we’ve partnered with Sylvia Garcia to do a few vaccine clinics in local churches. We’re taking vaccines out of the clinic to where people actually are and can regularly access services, which is one of the only real ways to really expand distribution.
What are some challenges these groups face?
It starts out with figuring out where you can get a vaccine and early on if you even qualified was difficult to navigate.
For a lot of my more multigenerational families, a lot of kids were tasked with figuring all that out for the parents. It also goes on to transportation: How are you going to get to the site? Also, who are you going to follow up with if you have symptoms afterwards, if you’re not an established patient with Legacy?
Not only are there those barriers, but there is also a lack of established trust with the healthcare system before the pandemic started. If you aren’t getting regular healthcare you probably aren’t used to getting messages about vaccines, comfortable with getting vaccines, and being told what to do with your health.