“We weren’t really set up for video with patients prior to this,” Dr. Jessica Dean said. “We all had some pretty rapid learning to do to have everything approved legally.”
Plummeting patient volumes as a result of the pandemic spurred rapid adoption of telemedicine, which has since become the new normal of health care, said Neil Simon, chief operating officer for eMDs, a company in Richardson that responded to the crisis by augmenting its medical practice software with telehealth capabilities.
“Telehealth was always something that was in the industry, but it was still very limited and had never really taken off the way people thought it would,” he said. “Once a lot of these business closures came down, [doctors] recognized they needed a way to see their patients.”
Less than a quarter of the nation’s health care organizations had an existing virtual care program as of January 2020, according to market research firm Forrester. By the end of this year, telehealth appointments are projected to surge to at least 1 billion. Ninety percent of those visits, Forrester projected, will be related to COVID-19.
Doctors were slow to use the technology for several reasons, but perhaps the biggest driver was unequal reimbursement, said Alex Edsel, digital marketing professor at The University of Texas at Dallas.
“The biggest thing that has been suppressing telemedicine all along has been the fact that, up until recently with this COVID thing, physicians were not getting paid the same as an in-person visit,” he said.
In late March, The Centers for Medicare and Medicaid Services responded to calls from struggling physicians by allowing 85 telemedicine services to be billed at the same rate as in-person visits. Many private insurers quickly followed suit, Edsel said.
Because of this change, doctors could turn to virtual care as a source of much-needed revenue, Simon said.
“Once the physicians recognized that what they were getting paid for a televisit was very similar to what they were getting paid for an office visit ... they were able to pick their [patient] volumes back up,” he said.
By late March, Dean said her office was seeing a majority of patients virtually. Her practice is expected to log more than 25,000 visits in May, which is about 80% of the appointments held pre-COVID.
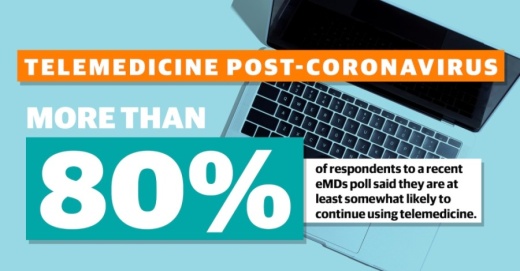
There was a slight learning curve at first, but Dean said she now sees virtual care as a necessary service. According to a recent poll of 175 eMDs software users nationwide, more than 80% say they are at least somewhat likely to use telemedicine moving forward.
“This is thrusting us all into that televideo universe,” Dean said. “I think just about every doctor would like to be able to have that option for patients.”
Many patients have also become accustomed to virtual visits and will likely demand more convenient access to care once the pandemic is over, Edsel said.
“It’s not for everybody, but now a huge swath of people like the convenience of it,” he said “There’s going to be a huge chunk of patients that are going to start pushing telemedicine.”
The long-term prevalence of telehealth will hinge on changes to reimbursement, Edsel said. But now that the floodgates have opened, it will be impossible to return to the way things were before.
“I don’t know if it’s the new normal—I think it’s too early to make that prediction,” he said. “What we can say is the adoption rate will increase significantly”
Simon predicts the future of health care will include a combination of both office and virtual visits.
“We will have a new normal that we all get used to,” he said. “It won’t be exactly what it was before, but I don’t believe what we have today is what it is going to be forever.”