As of July 14, nine cases have been confirmed in Travis County, while eight more are presumptive.
“Monkeypox is a virus that is creating illness in our community and a growing concern,” said Dr. Dessmar Walkes, Travis County health authority.
Monkeypox is spread by contact with bodily fluids, which can include through sex, touching skin lesions or touching items that have been exposed to the infection, according to Walkes. The symptoms include a pimple-like rash, fever and chills.
Walkes said the disease typically lasts around 21 days.
Dr. Kristin Mondy, chief of the Division of Infectious Disease with the University of Texas Dell Medical School, provided a few examples of how the infection can spread, including through sharing utensils and beverages, skin-to-skin contact, bodily fluid getting splashed on another person or touching bedding of an infected person.
She said those who are infected can also worsen their own infection by touching lesions and then touching other parts of their body, such as rubbing their eyes or putting in a contact lens.
Mondy said anyone cleaning contaminated surfaces should wear a mask, gloves and eye protection.
Monkeypox can remain on a surface for up to 15 days after exposure, Walkes said.
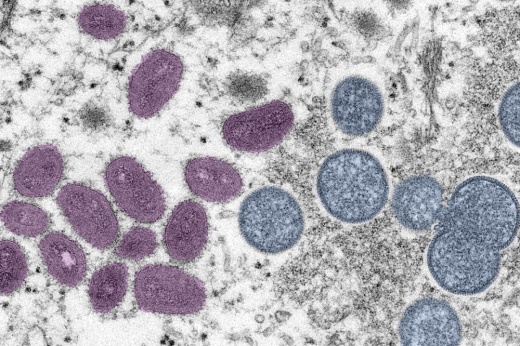
Monkeypox has two strains—West African and Central African, according to Mondy. She said the West African strain that is spreading in the United States and that it is the more mild of the two.
She said only 1% of those who are infected die.
The disease caused by the infection can be more severe for children under 8 years old, pregnant women and those who are immunocompromised, Mondy said. The infection can spread from a pregnant person to their fetus and cause miscarriage, Mondy said.
The case can also be more severe if the level of exposure is higher or depending on the area of the rash, Mondy said. Some examples she gave include individuals who get the infection in their mouth could be at risk for conditions such as pneumonia, or extreme cases could have difficulty eating.
APH Director Dr. Adrienne Sturrup said individuals need to make precautions with understanding the health history of someone they have sex with.
Mondy said those who are infected have a responsibility to treat their lesions as contagious until they are entirely healed—which can take several weeks—and use condoms for 12 weeks after infection.
APH is not offering mass-testing opportunities, but it is working with the state to test on a case-by-case basis. At this time, it is only offering vaccines for those who have been in close contact with an infected person.
Monkeypox is not related to chickenpox, Mondy said, so past chickenpox infections do not impact a person’s risk of monkeypox. However, it is possible someone who received a smallpox vaccine may have some immunity to the infection depending on how long ago the vaccine was administered.
Walkes said both testing and vaccination efforts can be ramped up if the spread increases.
Dr. Michael Stefanowicz, sexual health director with Community Care, said it is important to understand that while the disease is having a disproportionate effect on gay and bisexual men, it is not limited to the LGBTQ community.
“Monkeypox is not a disease of the gay community,” Stefanowicz said.
Williamson County announced its first presumptive case of monkeypox July 14.