“That was before the layoffs, so now the phones are ringing off the hook,” Simmons said.
TOMAGWA is a safety-net clinic providing care to those ineligible for or unable to access health insurance, Simmons said. The nonprofit’s reach spans 16 ZIP codes throughout portions of Harris, Montgomery and Waller counties, six of which are located in Community Impact Newspaper's Spring and Klein coverage area. The organization serves about 3,000 patients annually.
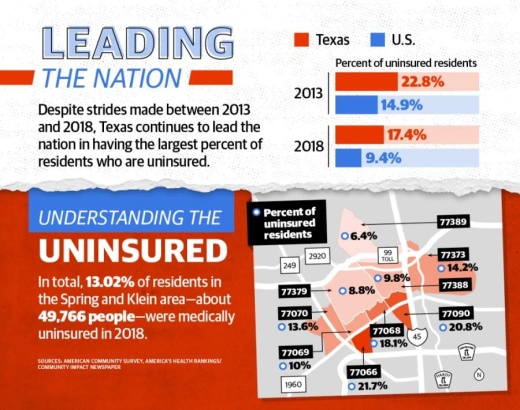
More than 49,700 residents within the Spring- and Klein-area's nine ZIP codes are uninsured, according to 2018 five-year estimates from the U.S. Census Bureau—about 13% of the area's total population.
“That’s what keeps me up at night is fighting tooth and nail every day to be a voice for the population we serve, the uninsured citizens in our area, so they can have access to care,” Simmons said.
During the pandemic, Simmons said it is crucial that the most vulnerable populations have access to health care and free coronavirus testing to stay healthy, avoid flooding emergency rooms and limit the spread of the virus. Other than community clinics such as TOMAGWA, the only other health care option for the uninsured is the emergency room, she said.
"One of our roles as a federally qualified health center is to keep people out of the emergency room for nonemergency issues, and that's particularly important during the COVID-19 pandemic," said Kevin Nix, the vice president of communications for Avenue 360 Health & Wellness, which has seven locations in the Greater Houston area, including one in Spring to treat those who are medically uninsured.
However, Brian Carr, the chief advancement officer of Northwest Assistance Ministries, which operates a full-service pediatric clinic in Spring, said fear of exposure has led many families to forgo routine preventative health care measures, such as vaccinations, which he said could have detrimental long-term effects.
"I think that element of fear is going to have some trickle-down effect over the next few months, even years, if they skip vaccinations and their immune system gets brought down to dangerous levels," Carr said. "We have the safety protocols in place to protect families, to protect their children from exposure, and so there’s just no reason to neglect every day health concerns during this time."
Carr added while the pediatric clinic has experienced a decrease in patients due to COVID-19 concerns, the clinic has simultaneously experienced an increase in patients who have no medical insurance.
"What we have seen with the patients that are showing up is a lot more patients that don't have any type of insurance, maybe because ... one of them lost a job or has been laid off or furloughed due to the coronavirus," Carr said.
Counting the uninsured
Texas leads the nation in having the largest percentage of residents who are uninsured. Census estimates show 17.4% of Texans were uninsured in 2018, down from 22.8% in 2013. This totals 4.76 million Texans in 2018 who did not have health insurance. Locally, the Spring- and Klein-area's uninsured population dropped from 18.2% in 2013 to 13% in 2018.
By comparison, the U.S. rate dropped from 14.9% to 9.4% from 2013 to 2018, according to census estimates.
“One of the challenges we have in Texas is we’ve got a lot of small businesses, a lot of independent contractors. These businesses struggle to provide health insurance. If you’re an independent contractor, it’s hard for you to be able to afford health insurance,” said John Hawkins, senior vice president for advocacy and public policy with the Texas Hospital Association.
Texas also has the second-highest noncitizen population behind California, totaling 2.96 million individuals, nearly half of which were uninsured in 2018, according to census estimates.
Health care and policy leaders also point to Texas’ hesitancy to expand Medicaid eligibility—as outlined by the Affordable Care Act—as a contributor to the state’s large uninsured population. According to a report from the Kaiser Family Foundation, 1.5 million currently uninsured, nonelderly adults could be covered if the state expanded Medicaid eligibility.
Six of the nine ZIP codes in the Spring- and Klein-area fell below Texas’ uninsured rate in 2018, but only ZIP codes 77379 and 77389 fell below both the state's and nation’s uninsured rate in 2018 with 8.8% and 6.4% of residents uninsured, respectively, according to census estimates.
By comparison, the uninsured rates for ZIP codes 77066, 77068 and 77090 each surpassed both the state and national rates at 21.7%, 18.1% and 20.8%, respectively.
Simmons said many of her patients are among the retail and food service workers as well as small businesses for which paying for or providing health insurance is difficult.
“Most of our patients are in those industries who had to do the layoffs, and so they are finding themselves without insurance—or even before [the pandemic] they could not afford it so they relied on safety-net clinics like TOMAGWA,” Simmons said.
A growing rate
Data from the Texas Workforce Commission shows 1.96 million unemployment claims were filed in Texas between the weeks ending March 14 and May 2.
Locally, about 9% of the labor force in Spring and Klein filed for unemployment in the month spanning March 25-April 25, according to census and TWC estimates.
A May 13 report from the Kaiser Family Foundation projects 382,000 Texans will be within a coverage gap—meaning they will be unable to access health insurance—in January 2021, when employer-sponsored insurance and unemployment insurance benefits are likely to run out. This is up from the 30,000 Texans projected to be in the coverage gap in May because of job loss.
To prepare for an influx of uninsured residents locally, Simmons said TOMAGWA is moving its enrollment process online. By May 26, TOMAGWA will roll out its online system, where patients can fill out forms to be approved virtually, and then health assessments will be done in person and scheduled daily. Previously, prospective clients had to have lengthy visits with TOMAGWA staff and doctors to become a patient, Simmons said.
TOMAGWA is also primarily using telehealth services to care for its patients except the chronically ill, who are still being seen in person by appointment. Telehealth has allowed the nonprofit to see patients more efficiently and conserve personal protective equipment, Simmons said.
“For us, because our focus is the rural areas where there is just a lack of access to health care, period—even for the insured—if the insured struggle with access to health care, imagine things without insurance,” she said.
Likewise, Avenue 360 Health & Wellness has also taken this pandemic as an opportunity to launch its telemedicine initiative in March and streamline its patient registration process in preparation.
"We've made it a lot easier for patients to get registered and be able to be seen by a provider ... by working on our website and our patient portal," said Dr. Therese Obioha, regional medical director for the Spring location of Avenue 360 Health & Wellness. "A lot of it can be done electronically [now] and patients seem to find a lot of relative ease with it."
Care during COVID-19
Simmons said caring for the uninsured is particularly difficult because of limited funding, a lack of PPE and few COVID-19 testing resources close by for the uninsured population.
Simmons previously said TOMAGWA has seen financial contributions slow significantly amid economic effects of the coronavirus. The same could be said for NAM, which Carr said relies on grant funding, corporate and community donations to keep its pediatric clinic running.
While NAM and Avenue 360 have been able to provide coronavirus testing throughout the pandemic, Simmons said TOMAGWA has not been able to access COVID-19 testing kits, perhaps the largest need in caring for the uninsured community currently.
“That’s the big issue,” she said. “As a safety-net clinic we are not on any list to receive COVID-19 tests, so we have to get out there and fight just as an individual practice to get access to the tests. So far we’re still unsuccessful, so that leaves the uninsured population without a place to go or receive tests.”
Some testing sites have been set up around Harris County, however, Simmons said not having transportation is the No. 1 barrier for the uninsured population to receive health care.
“Without them having the resources—the money to pay for tests—without them having their safety-net clinic being able to provide the test, you have this large population of people who are not tested who can be spreading the virus and making it worse,” Simmons said. “I think that will continue to be a barrier in our ability as counties to manage the spread because we have not made it accessible for uninsured residents in the rural areas to have consistent access to testing.”
For more information on which options are available to those who are uninsured, click here.