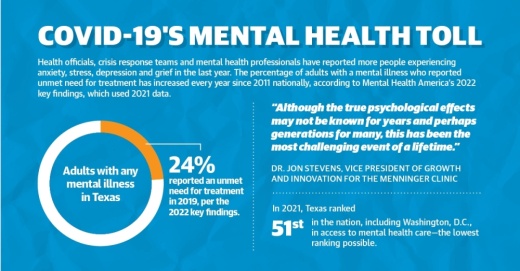
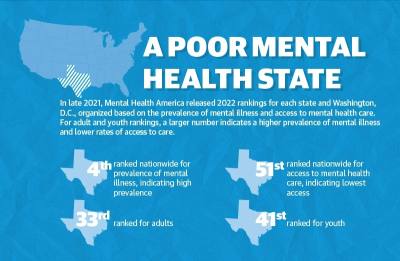
Mental Health America’s 2022 key findings, which use 2021 data, organized each state and Washington, D.C., based on mental illness prevalence and access to mental health care. Texas ranked 27th overall, but was third in terms of prevalence of mental illness and 51st—the lowest possible—for access to care.
Local experts said access to mental health care has been an issue in Texas since long before the pandemic. In 2017, Mental Illness Policy Org. reported the state allocated 1.2% of its total state expenditures to mental illness; this compares with states on the higher end of spending, such as Arizona, Pennsylvania and Maine, which allocated 4.8%-5.6% of their expenditures to mental illness.
“Unfortunately, the mental health care system[s] in Houston and Texas proper were already inferior to many other states prior to the pandemic,” said Dr. Jon Stevens, vice president of growth and innovation for The Menninger Clinic, a Houston psychiatric facility. “Although the true psychological effects may not be known for years and perhaps generations for many, this has been the most challenging event of a lifetime.”
Officials with mental health centers in Harris and Galveston counties said COVID-19 has exacerbated the anxiety and depression already present among residents as well as put even more strain on already understaffed clinics. Telehealth has improved access for some patients, and providers point to group support as a potential path forward for those hoping to improve their mental well-being.
Skyrocketing demand
Across the Bay Area, mental health providers and experts said the pandemic has underscored the need for more services as demand climbs.
The Harris Center for Mental Health and Intellectual and Developmental Disabilities supports about 60,000-80,000 primarily underinsured or uninsured patients annually, offering outpatient services and crisis intervention. Over the past 18 months, officials said they have seen an increase in the demand for services.
According to data from The Harris Center, the center’s crisis line has seen a 58% increase in callers since April 2020 who presented symptoms, concerns or suicidal ideation requiring a telephonic mental health assessment as well as a 34% rise in calls from county residents via the National Suicide Prevention Lifeline, which is answered by The Harris Center crisis line.
Prolonged isolation, economic challenges and delaying seeking treatment due to COVID-19 concerns have contributed to the spike, said Luming Li, who joined The Harris Center as chief medical officer in August.
In Galveston and Brazoria counties, the Gulf Coast Center serves as the local mental health, intellectual and developmental disability authority as well as a substance use recovery provider.
CEO Melissa Meadows said via email the center implemented a crisis counseling program designed for those in need of no-cost emotional support caused by the pandemic. From August 2020 to early December 2021, the program served 1,348 individual participants and 1,377 group counseling participants, she said.
The center also provided Mental Health First Aid courses to help participants learn to recognize when someone needs emotional support or mental health services, she said. Gulf Coast Center gave 29 trainings in Galveston County from fall 2019 to fall 2021.
Meanwhile, UTMB Health has four Bay Area locations that provide mental health services: two in Webster and two in League City. While patient volume has remained steady during the pandemic, clinics are limited based on the number of providers and their caps on caseloads, UTMB officials said.
UTMB Health Psychiatry Webster on Texas Avenue saw about 9,900 patients from September 2019 to August 2020; that number increased nearly 20% to about 11,800 patients seen from September 2020 to August 2021, according to UTMB data.
Telehealth has enabled many patients to seek treatment from the safety of their homes, although it does not come without challenges, Li said. While the introduction of telehealth has opened doors in terms of access, the demand is greatly outpacing the number of providers available for counseling, said Jeff Temple, a professor and licensed psychologist at UTMB.
“There’s only so many hours and only so many people that an individual [provider] can see,” Temple said. “The increased access has helped, but the demand is so great that it still is leaving people lacking.”
COVID-19 stressors
The uncertainty of the pandemic combined with other major events, such as the February freeze, has created conditions that many are unable to cope with on their own, Temple said. He and Dwight Wolf, medical director for UTMB Health’s psychiatry and behavioral services outpatient clinic, said anxiety and depression among area patients have dramatically increased throughout COVID-19.
Burnout is a real possibility for providers as they try to tackle patients’ varying needs, whether remotely or in an office. Li said the pandemic has taken its toll on providers’ mental health, leading to retention challenges.
“I could hire 10 psychologists, and they’d probably be full in a couple of months,” Temple said. “The demand is there. ... The providers just aren’t there.”
Many people wait until they are in crisis to seek help, resulting in a need for immediate intervention, and behavioral therapy is best provided in person, Meadows said. The increased stress and vulnerability people are feeling have led to higher incidents of crisis, she said.
Li said the same is happening in Harris County.
“Maybe [people] didn’t seek care early enough or they waited for a while until their condition got significantly worse, so they’re coming in at a worse state than what we were seeing pre-pandemic,” Li said.
According to Meadows and Galveston County Health District CEO Philip Keiser, the county has seen a rise in opiate-associated deaths and substance use during COVID-19.
Keiser emphasized substance use disorder clinics are needed now more than ever, and existing clinics can barely meet current needs. For those seeking mental health treatment, waitlists are long, Keiser added.
“If people have mental health issues, there are very few options for them if they don’t have money and insurance,” he said. “Quite frankly, there’s not a lot of options for people even if they do.”
Group support
Providers in Harris and Galveston counties said they are hopeful that community-centric interventions, from group therapy to support phone lines, can play a role in helping residents make sustainable changes to their mental health moving forward.
Community Health Network Systems, which operates hospitals and outpatient care centers nationwide, opened a League City campus in fall 2019. The patient load has increased by 30% in its two years of operation, per CHN data: About 6,350 patients were seen from fall 2019 to fall 2020, compared to more than 9,000 from fall 2020 to fall 2021.
Providers have added more support groups over time, in which patients can talk through issues alongside others going through the same experiences, said Veronica Cavazos, one of the campus’s behavioral therapists.
More than a dozen options are now available virtually and in person through the CHN campus in League City. New groups were added as recently as October based on the need, Cavazos said.
“We have a lot of resources and a lot of access for patients in whatever situation they may be in—we’re here to help,” she said.
While telehealth is not a perfect system, she said the ability to provide care without a patient needing to travel to an office has been critical in ensuring access. The use of the campus’s virtual services skyrocketed after the pandemic started, Cavazos said.
“I think it was a really, really huge lifeline for many people,” she said.
Additionally, UTMB has a text-based support service in which subscribers receive three weekly messages. Temple said these can be useful for substance use tips and motivational tips.
Gulf Coast Center provides services through the statewide Military Veteran Peer Network. Virtual groups throughout the pandemic have been a positive addition to providing accessible social support to the veterans the center serves, Meadows said.
The Harris Center received about $15.9 million in COVID-19-related state and federal funding in fiscal years 2020 and 2021, which was in part used to establish a COVID-19 mental health support line, Director of Communications Karen Boren said.
“This was a direct response to COVID-19 just because we saw an influx in mental health-related crisis calls to our crisis line,” Boren said.