The project stems from a 2018 bond election Tarrant County voters approved with 82% of the vote. Once completed, the project will have breathed new life into the JPS Hospital’s main campus and created a new hospital complex adjacent to its current location to help better care for patients needing mental health services.
“With this new psychiatric emergency center, JPS will be able to redefine our points of mental and behavioral health access and support the growing health care needs in Tarrant County,” JPS President and CEO Dr. Karen Duncan said during the center’s groundbreaking ceremony Oct. 26.
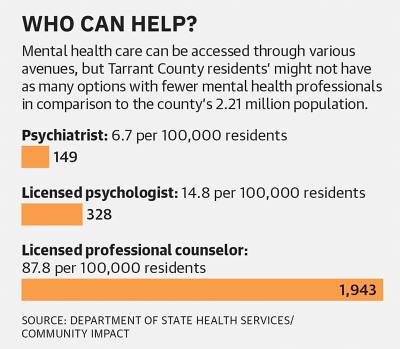
The hospital system increasing its access to care comes as hospitals have little capacity for mental health patients and the region faces a shortage of mental health care professionals.
All Texas Access, a legislatively directed initiative that focuses on increasing access to mental health services, found in its 2022 report that North Texas needs additional crisis beds as well as inpatient psychiatric beds.
Project details
The main John Peter Smith Hospital campus is located at 1500 S. Main St. in Fort Worth. JPS Health Network serves all of Tarrant County and has clinics located in Grapevine, Fort Worth, Euless and surrounding areas. Nearly 40% of the hospital’s operating budget is from property taxes collected in Tarrant County, according to its 2021-22 fiscal year budget.
The project’s $1.5 billion price tag will be split between sold bonds and operating cash from JPS.
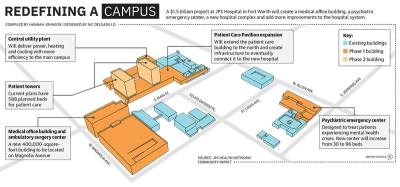
Phase 1 of the project—set at $635 million—includes a new ambulatory surgery center, medical office building, psychiatric emergency center, parking garage, central utility plant and transitional parking around the main campus for construction. The first phase will also build the Medical Home Southwest Tarrant facility, which will be a primary care clinic.
These projects will be funded with $450 million in bonds and $185 million in operating cash. Phase 1 is projected to be completed between 2025 and 2027, according to JPS.
The second phase of the project is estimated to cost $876 million and finishes out the program with new inpatient towers that will connect to the Patient Care Pavilion. The second group of bonds, expected to be sold in late 2026 or early 2027, will be $350 million. The remaining portion of the project will be paid for with $526 million in cash, according to JPS.
“The ... bond program will allow JPS Health Network to develop modernized and much-needed facilities at both Main Campus and in southwest Tarrant County, ensuring the residents of Tarrant County have access to excellent care for the next 50 years and beyond,” said Jessica Virnoche, a JPS spokesperson, in an email.
While approved by Tarrant County voters in 2018, the first group of bonds for Phase 1 were not sold until February 2023. In addition to the COVID-19 pandemic delaying the start of the bond program, Virnoche said the network had to take time to plan the project and its phases. JPS sought feedback from doctors, nurses and team members on the vision for the project.
•Residents were able to give feedback through an online survey on how the future facilities could meet the community’s needs.
“Prioritizing and staging all of the projects that are contemplated by the program requires a lot of discussion and planning that is not easily visible but is a necessary part of the work,” Virnoche said.
JPS broke ground on the new psychiatric emergency center Oct. 26. The new facility will increase capacity from 30 beds to 96 beds and will address a “critical short-term need,” according to JPS officials.
“[The psychiatric center] will be a very critical tool that we’re improving on in that tool box of how we work with folks with mental health issues,” former Tarrant County Judge B. Glen Whitley said at the groundbreaking ceremony.
The current center is located on the 10th floor of the hospital’s main campus. JPS’ new center will be attached to the network’s current inpatient behavioral health hospital, at 1600 May St. in Fort Worth, which will allow for a “smooth continuum of care,” Virnoche said.
Filling the gap
JPS operates Tarrant County’s only psychiatric emergency center.
The center provides services for voluntary and involuntary patients in mental health crises, such as severe symptoms of depression, anxiety or other conditions that are difficult to control.
While there are no mental health hospitals in the cities of Grapevine, Colleyville and Southlake, the closest available resources are Methodist Health System’s psychiatric inpatient hospital at its Richardson facility and Texas Health Resources’s Behavioral Health Hospital in Arlington. Help can also be found at My Health My Resources of Tarrant County which aids in providing mental health resources to people in the county who are uninsured.
According to JPS, its current facility is among the busiest psychiatric hospitals in the nation, providing treatment for adults and teens with psychiatric illness—averaging 20,000 patients a year.
Part of this growth in demand comes from the COVID-19 pandemic, according to Tiffany Young, a spokesperson for the Texas Health Human Services Commission.
“The COVID-19 pandemic created a steep rise in anxiety, depression and stress across the state, and an unprecedented demand for mental health services,” Young said in an email.
Most North Texas counties are designated as mental health workforce shortage areas, Young said. A health professional shortage is identified by the U.S. Department of Health and Human Services. A shortage area is an area, population or facility experiencing a shortage of providers for primary care, dental or mental health care, she said.
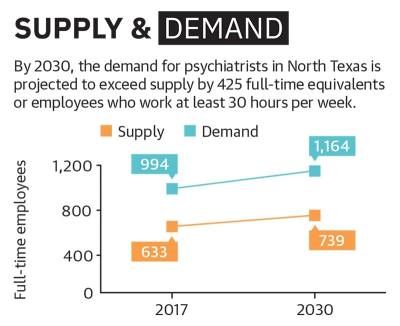
The supply and demand for psychiatrists are both projected to grow by about 17% between 2017 and 2030 in North Texas, according to a study by Texas Department of State Health Services. This number is determined by full-time equivalents, or FTEs, which measure how many full-time employees a business needs to operate.
While the supply is projected to grow, the demand will exceed supply with the shortage of psychiatrists increasing from 361 to 425 employees by 2030.
“North Texas ... faces a shortage of mental health professionals, and the Texas Health and Human Services Commission is working with [local mental health authorities] and their partners to meet the mental health needs of communities,” Young said.
Cody Thorn contributed to this report.