Data from St. David’s healthcare facilities in Central Texas shows the number of telehealth visits were up nearly 3,000% in 2021 compared to 2019.
National figures run parallel to local data, as a recent snapshot from the Center for Medicare & Medicaid Services indicates an approximately 3,000% increase in the number of telehealth sessions held nationwide from March 2019-March 2021.

Providers in Round Rock, Pflugerville and Hutto also saw stark jumps in telehealth visits in the last two years, and local health care professionals agree that virtual care will remain a popular choice for patients when available.
“I just don’t think any of us are going to ever want to revert back—as patients and even as providers,” said Tiffany Berry, vice president of primary care at Baylor Scott & White Health.
Advantages and disadvantages
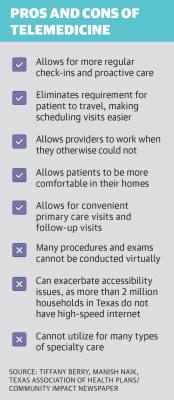
Berry said while virtual health care is not without its limitations, it has many applications beyond social distancing.
Convenience, both for patients and for providers, is one of telemedicine’s greatest strengths, she said.
Round Rock resident Ellen Leary, who since 2020 has used telehealth for regular doctor visits, filling prescriptions and postpartum psychiatry, said the option to meet with a doctor virtually makes those visits much easier.
“It’s convenient, for sure—being able to work around my schedule instead of having to find an appointment at a doctor’s office and find child care,” Leary said.
Telehealth also allows health care professionals to work when circumstances might otherwise prevent them from doing so, which helps providers deliver a more consistent level of care, according to Berry.
“If they’ve got a sick kid or they’re not feeling well themselves—still feeling good enough to work, just don’t want to expose patients—it gives our [advanced practice providers] and our physicians more flexibility to still be able to take care of people, just to do it from home,” Berry said.
However, Berry said while telehealth can be a valuable tool for primary care, some specialty areas such as orthopedics and rheumatology require procedures or thorough exams that can only be conducted in person.
Manish Naik, a doctor at Austin Regional Clinic, said the technology itself presents its own set of challenges.
Physicians, nurses and patients have all had to learn how to use new technology, he said, which has created an additional barrier to receiving and providing care.
Further, Naik said, not every patient has access to high-speed internet or a device that can use it.
“Video just doesn’t work as well without a reliable connection,” he said.
Widespread use
Regional health care networks including Baylor Scott & White and ARC have been eager adopters of telemedicine. As one example, in Central Texas, telehealth visits within the St. David’s network of providers went up about 4,660% from 2019-20 because of the COVID-19 pandemic, according to the health care provider.
But the utilization of virtual medicine also extends to smaller practices, mental health care and even school health offices.
Professional counselor Kinga Kasprzyk runs a Round Rock-based virtual therapy practice called Courageous Conversations Therapy.
Kasprzyk started her practice in June 2021, offering only virtual sessions out of necessity. However, she said she plans to continue operating fully virtually for the foreseeable future.
In addition to the convenience factor, Kasprzyk said her clients often feel more comfortable speaking with her from their own homes.
However, Kasprzyk said the technology issues that come with telehealth can be especially disruptive in the case of mental health care.
“Maybe somebody’s revealing something for the first time to you, or they’re really vulnerable and they begin to cry, and then all of a sudden the session cuts out because your Wi-Fi goes out or whatever,” she said.
As another example, Hutto ISD has partnered with a school telehealth company called Hazel Health to provide virtual services for students across its 10 schools.
District information states the program allows nurses at Hutto schools to connect students virtually with a doctor or nurse practitioner when their needs exceed the capabilities of the school health office.
Julie Swed, the nurse at Hutto Elementary School, said the partnership with Hazel Health means she can more effectively provide care for students who might otherwise need to leave school for a doctor’s appointment.
“Before Hazel ... either the kid has to tough it out at school the rest of the day without much relief, or a parent has to take off work early, come pick them up [then] make a doctor’s appointment,” Swed said.
The future of telemedicine
As new technology continues to develop, Berry said she expects the applications of telehealth to expand further in the coming years.
One application Berry said she is excited to explore is chronic disease management, something that will be aided by the use of peripherals, or testing devices for things like blood pressure that patients keep at home.
“When you’re coming in every three months, or even once a month or more ... it just fills your life,” Berry said. “A quick video visit ... is just a game-changer.”
Naik said he does not expect demand for virtual health care to diminish, and health care providers should be prepared to adapt as new developments arrive.
“I think it’s up to us as health care providers to continue to more effectively leverage technology,” Naik said.