One year after the first coronavirus cases were detected in Texas, thousands of health care workers and vulnerable Texans have been inoculated with a vaccine for COVID-19 that was developed in record time.
As the local effort to vaccinate as many residents as possible continues, health officials and city and county leaders have been working together to improve the process.
“Partnerships are a big deal. We couldn’t do what we do without our city partners,” said Gentrea Hendrickson, the public health emergency preparedness coordinator for the Comal County Public Health Department. “The more partnerships you build, the easier and the quicker it is to start moving towards that mass-vaccination model.”
In that spirit, the last several months have served as a guide for how to improve the process, according to many area health care professionals. Despite the fact that severe winter weather in mid
February caused temporary power outages and a loss of running water for many in the community, the local vaccine rollout remained largely unaffected, according to local officials.
By March 1, 18,493 Comal County residents had received at least one dose of the vaccine, while 5,718 had received both doses, according to the Texas Department of State Health Services. In Guadalupe County, 13,660 residents had been given at least one dose and 5,170 had been fully vaccinated.
“Right now we don’t have a specific dedicated treatment to get rid of this virus,” said Dr. Emily Briggs of New Braunfels-based Briggs Family Medicine. “And so, if we can prevent it from getting to somebody’s body, well, that’s the thing to do.”
Early rollout turbulence
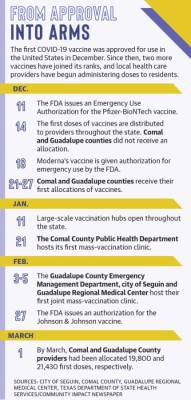
In December, the Food and Drug Administration issued an Emergency Use Authorization for the Pfizer-BioNTech and Moderna vaccines.
The first allotment of vaccines arrived in Texas the week of Dec. 14 and was distributed to hospitals and medical centers throughout the state to be administered to health care workers and frontline workers.
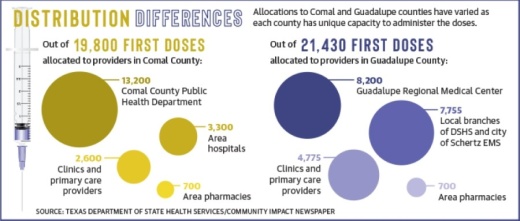
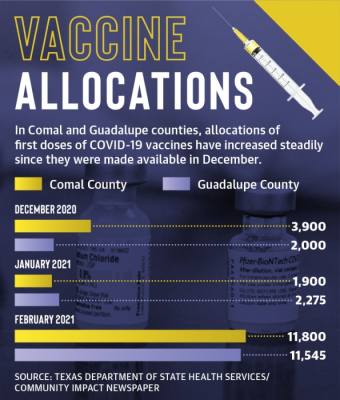
During the week of Dec. 21, 3,900 doses were delivered to Comal County hospitals and clinics, while Guadalupe County providers received 2,000 doses, according to DSHS. By the beginning of March, Comal County had received 19,800 first doses and 10,700 second doses, while Guadalupe County has been allocated 21,430 first doses and 11,545 second doses.
Ahead of the FDA’s decision to approve both vaccines for emergency use, health care providers and public health officials enrolled in the Vaccine Allocation and Ordering System, which is run by the DSHS, according to Hendrickson.
Once enrolled in the system, providers gave evidence that they would be able to accommodate the cold storage needed for both vaccines and submitted orders for approval by the state vaccine emergency advisory panel, Hendrickson said.
“It was at first a very benign process. The state asked, ‘Hey, would you be willing to give the vaccine when we have a vaccine?’” said Dr. Emily Briggs of Briggs Family Medicine.
Briggs is one of 56 providers in Comal County who expressed interest in administering the vaccine and one of 16 who the panel approved to receive doses.
On Dec. 21, Briggs and 10 other hospitals, clinics and pharmacies in the county were allocated doses, but she said the process was anything but smooth at the beginning of the vaccination effort.
“The vaccine just showed up on our porch,” Briggs said. “It arrived [on Dec. 23] when offices would have been potentially on vacation. And thankfully, they were not.”
Of the 11 providers who received shipments, three primary care offices in New Braunfels received a combined 600 doses, according to the DSHS allocation records. Briggs Family Medicine received 100; Christus Trinity Clinic received 200; and Madison D. Lowry MD received 300.
Lowry’s office had to temporarily stop seeing patients in order to administer vaccines as quickly as possible after they arrived, Briggs said.
“It was a godsend to our community that he was able to vaccinate so many health care providers and then some that were over the age of 65,” she said. “It was beautiful, but his practice took a hit because of it.”
In early January, the state shifted its focus to administering immunizations through large-scale hubs and providers that could conduct mass-vaccination events.
Though it is not a registered hub location, the Comal County Public Health Department partnered with the city of New Braunfels and Galen College of Nursing to create a vaccination center at the New Braunfels Civic/Convention Center.
The department used the first event to demonstrate to state officials its capacity to vaccinate hundreds of people in a single day without significant delays while also filing the necessary paperwork to the state, Hendrickson said.
After two weeks of successfully administering 500 doses at the vaccination center, the public health department began receiving weekly regular allocations of 2,000-4,000 vaccines. Despite the uptick, many have struggled to secure spots on the waitlist as demand continues to outpace available vaccines.
For Renea Tutt, a New Braunfels resident who has an autoimmune disorder, securing a time slot to be vaccinated required patience and regular checks to the Comal County website.
“I would keep checking the websites periodically to see if there were any slots available,” Tutt said, adding that when she finally got an appointment to be vaccinated at the civic center on Feb. 4, the process was smooth and faster than expected.
Guadalupe County rollout
Early vaccination efforts in Guadalupe County were similar to neighboring communities after the first allocations went to the Guadalupe Regional Medical Center and local pharmacies, but the area has struggled to secure large weekly shipments.
In Schertz, the city’s emergency medical services department has been receiving regular shipments since the week of Jan. 4, but because the county does not have a public health department, it was difficult to conduct mass vaccinations in other parts of the county, according to Seguin City Manager Steve Parker.
On Jan. 20, the Guadalupe County Emergency Management Department, the city of Seguin and the GRMC submitted a proposal to the DSHS to create three vaccine hubs in the county with the capability of providing 1,000 vaccines per day.
After weeks of waiting, the vaccination center was allotted 5,000 doses of vaccine during the week of Feb. 1, though its hub designation is still pending.
“We felt really prepared when we got our 5,000,” Parker said. “This would be a really good thing, so we start off with 1,000 doses the first day, just trying to make sure we got our feet wet.”
Vaccinations were administered to eligible residents Feb. 3-5 at the Seguin Coliseum where nurses, volunteers and retired health care professionals gave shots and recorded data for the state system.
Since the week of Feb. 1, the collaborative effort has continued to receive doses, though the allocations have not been consistent in size.
“I think, honestly, one of the biggest challenges is just supply—the supply isn’t there,” said Sheri Williams, chief operations officer for GRMC. “And then, [it is difficult] maintaining the ability to have enough volunteers to run these vaccine clinics.”
Light at the end of the tunnel
As local and state entities have worked to adjust their rollout efforts, nursing homes and long-term care facilities such as EdenHill Communities received vaccines through coordination between the federal Health and Human Services department and pharmacies including Walgreens.
Residents of these communities were identified as being particularly vulnerable to COVID-19 due to age and living in close proximity to others, according to Terry Jackson, director of independent living at EdenHill Communities. Because of those factors, residents and staff were prioritized in the state’s vaccination program.
“I just remember cheering when our CEO ran into my office and said, ‘We all got approved,’” Jackson said. “People screamed, just knowing that an end might be in sight to what we’ve all had to go through.”
On Feb. 26, Walgreens nursing staff administered the final second dose of COVID-19 vaccines to residents and staff at EdenHill. In total, approximately 90% of the 430 residents of the community are now fully vaccinated, along with 77% of the 297 staff members, Jackson said.
While efforts to streamline vaccine registration for members of Phase 1 of the state’s rollout continues, officials are beginning to plan for the next phase as supply slowly increases.
“It’s my hope that each month we get a little bit faster at opening up vaccines to people,” Hendrickson said.
Though the state has yet to specify the next group of eligible recipients, Johnson & Johnson’s one-dose vaccine may be approved as soon as early March.
Ultimately, while treatment practices for the virus are improving, prevention and vaccination are still the best hope for eventually ending the pandemic, Briggs said.
“This is a public health effort. This is not the time to be selfish; this is the time to recognize that we are in this together,” Briggs said. “As we are using science to combat this virus, we have so much more hope now than we ever had in 2020.”