The program provides faster, convenient and affordable access to medical providers for everyone—no insurance required. For $6 per month, billed as an opt-out fee on Garland’s utility bill, residents can connect with a doctor without sharing insurance information or paying a copay.
Accessible health care
TAP Telehealth was shaped by MD Health Pathways CEO and founder Dr. Dirk Perritt’s experience as an emergency medicine physician at a Garland hospital, where he saw the challenges patients face in accessing timely care.
TAP Telehealth gives residents direct access to ER-trained medical providers via text with no appointments, insurance hurdles or copays. For $6 per month, billed as an opt-out fee on Garland’s water utility bills, the program covers all household members, up to 10 people.
Once enrolled, residents can quickly connect with a licensed provider for guidance, prescriptions and follow-up care.
“We’re trying to put a doctor in every family so everyone has someone to text for medical help,” Perritt said. “About 97% of cases are resolved immediately, often with a low-cost prescription, and for those needing higher-level care or true emergencies, we guide them to the next step without leaving them on their own.”
How the program works
TAP Telehealth simplifies healthcare access for everyone, regardless of age or technical experience.
- Step 1: Start a visit. Residents text a dedicated TAP Telehealth number to begin. No app downloads or complicated logins are needed.
- Step 2: Connect with a licensed provider. Within minutes, a local provider evaluates the situation. Patients can describe symptoms, ask questions or send photos.
- Step 3: Receive guidance or treatment. Providers can recommend next steps, direct patients to in-person care if needed or send low-cost prescriptions to a local pharmacy.
“We designed this to be simple so families of all ages and language backgrounds can get care quickly,” Perritt said. “The service supports multiple languages, and if texting isn’t the easiest option, patients can switch to a phone or video call, ensuring everyone can access care in the way that works best for them.”
Why is this program necessary?
Garland, the largest U.S. city without a public hospital, has over 250,000 residents, 30% of whom are uninsured. Since early 2018, Garland residents have been without a hospital after Baylor Scott & White shut down due to financial losses.
Without a local hospital, many rely on emergency services for minor health issues, with ambulance trips to the nearest facility taking nearly two hours.
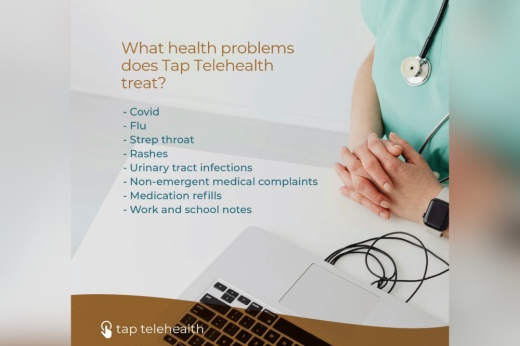
TAP Telehealth addresses this challenge while benefiting the broader community. By managing nonemergency cases virtually, the program frees up ambulances for true emergencies, helps keep children healthy and in school and allows adults to access care without missing work. It also reduces costly ER visits, lowers out-of-pocket expenses and ensures vulnerable residents have timely access to medical guidance.
TAP Telehealth is a citywide solution to improve public health, reduce strain on Garland’s emergency system and provide timely, accessible care to a community in need.
Garland’s citywide rollout of TAP Telehealth is scheduled for spring 2026, but residents won’t have to wait that long to experience it.
Starting in mid October, an early access pilot program will offer 10,000 Garland households free access to TAP Telehealth ahead of its full launch next year.
To be among the first 10,000 Garland families to try the TAP Telehealth program, click here.

To learn about TAP Telehealth, visit www.taptelehealth.com/garland for more information.
The above story was produced by Multi Platform Journalist Chloe Chapel with Community Impact's Storytelling team with information solely provided by the local business as part of their "sponsored content" purchase through our advertising team.