Emad Mikhail Bishai, a licensed psychiatrist and owner of The Woodlands Psychiatry and Counseling, said he has seen an increase in local patients seeking services over the past year.
“There is a surge of mental illness for sure,” Bishai said. “It has been on the rise for the past 20 years ... for depression, anxiety and suicide.”
In The Woodlands, law enforcement officers serving the township from Montgomery and Harris counties responded to 18 suicide and attempted suicide calls from June to September this year, making up nearly half of the 44 total reported so far in 2022, according to the quarterly law enforcement report presented to The Woodlands Township board of directors Oct. 26.
This follows a total of 58 suicide and attempted suicide incidents that officers responded to throughout 2021, according to reports presented in the annual law enforcement update in December 2021.
In Montgomery County, there has been a surge of mental health care cases this year as well. Montgomery County Precinct 1 Constable Philip Cash—who helps head the county’s mental health unit and crisis intervention team—told Montgomery County Commissioners Court in a midyear report July 26 the county had already surpassed the 4,765 calls it received in the entirety of 2021, and as of October, Capt. Brian Luly said in a phone interview that number had reached 8,185 for the third quarter.
The county expanded the unit in August 2021 with federal American Rescue Plan Act funding.
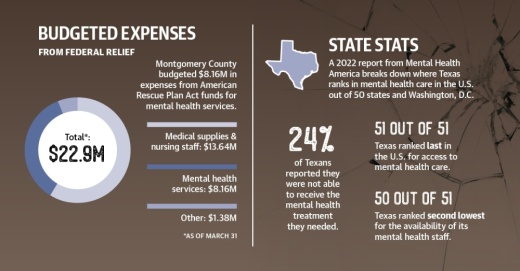
According to project and expenditure reports from the U.S. Department of the Treasury, Montgomery County budgeted $8.16 million, or more than one-third of its allocated funds for ARPA projects as of the final report date of March 31 , for mental health.of March 31, for mental health care.
Statewide, a 2022 report by Mental Health America ranks Texas last out of 51 states and territories for access to mental health care. As such, local groups, such as Montgomery County’s volunteer-based Behavioral Health and Suicide Prevention Task Force, said they are trying to improve access. The task force was created by Precinct 1 Judge Wayne Mack in 2020, according to previous reporting.
The task force began a gap analysis in September to determine what services are needed in the county, said Brenda LaVar, a member of the task force and president of the board of directors for the National Alliance on Mental Illness Greater Houston.
“When [families] can’t find help, that’s a real problem,” she said.
Uptick in mental health care demand
According to Cash’s report, calls for mental health services to the unit are projected to increase to 9,566 calls by the end of 2022, a 101% increase from 2021.
Officials said the most common category of calls through October were miscellaneous crisis intervention team responses, which consist of check-ins with citizens who have recently experienced mental health issues as well as those who recently completed outpatient visits with Tri-County Behavioral Healthcare, a federally qualified health center. Cash noted the ARPA funds have allowed officers to increase their follow-up frequency.
Meanwhile, Evan Roberson, director of Tri-County, which covers Walker, Montgomery and Liberty counties, said the mental health care provider saw 932 children age 5-17 who were in crisis from August 2021 to August 2022, surpassing the total in any previous year. In 2021, Tri-County had 761 child crisis cases.
However, as of Oct. 17, Roberson said Tri-County had 99 vacant positions out of a total of 460.
“We have made some progress, but we are still struggling,” he said. “This work is hard, and it has to be part of your makeup to really want to do this every day.”
Roberson said staffing shortages caused the center’s crisis stabilization unit to close in November 2021. People admitted to the 16-bed unit are generally uninsured and require hospitalization.
Roberson told commissioners Aug. 3 it would require nearly $2 million per year to restaff the program and pay competitive salaries, but he said he does not want to staff full-time positions using temporary ARPA funds. Further discussion is expected at a Nov. 8 Commissioners Court meeting.
“[Having those beds] is one of the biggest needs for this county, for law enforcement,” Precinct 3 Commissioner James Noack said Aug. 3. “Not having them is a disservice.”
Meanwhile, Roberson said in an October interview mental health care providers are concerned about the effect of an expected economic recession through the end of 2022.
“[This time] last year was very busy. I do not know what to expect this year,” Roberson said. “I have seen Decembers that are so quiet that nothing is going on, and you see other years where you are very busy. If I had to guess, we will be busy. ... On the horizon, though, is the potential for a recession.”
Barriers to access
In addition to staffing challenges, local organizations said lengthy waiting lists, a lack of providers and the cost of services are barriers to receiving mental health services in Montgomery County.
The area served by Tri-County is designated as a high-needs health care professionals shortage area for mental health, according to the U.S. Health Resources and Service Administration.
In addition, a 2022 report from Mental Health America shows there are 830 residents per mental health provider in the state, ranking Texas second lowest for provider availability in the U.S.
Locally, Ann Snyder, former president and CEO of Interfaith of The Woodlands, said she has seen an increase in advocacy, particularly for area nonprofits that provide mental health services, such as Mosaics of Mercy, which offers mental health and crisis services, particularly after the start of the coronavirus pandemic.
“It is important that we recognize the importance of people’s well-being,” said Snyder, a member of The Woodlands Township board of directors. “People appeared to be much more stressed and anxious about everyday life ... now in 2022. I think mental health is still being challenged, especially today with inflation and the economic conditions of our country.”
Sherry Burkhard, director of education for Mosaics of Mercy, said providers often have a waiting list for new clients.“
Since [the peak of the pandemic], our call volume has leveled out. ... But what we have seen is an increase in the complexity in calls and the difficulty in connecting to providers,” she said.
According to the NAMI, 43.4% of adults in Texas reported symptoms of anxiety or depression in February 2021, of which 26.4%—or 839,000 adults—were unable to get needed counseling or therapy with the cost cited as the barrier for 45.3% of those.
State Sen. Brandon Creighton, R-Conroe, said in an August email he expects the state to build upon its mental health funding in the upcoming legislative session, which will begin in January. He said the state invested $100 million in 2019 to create the Texas Child Mental Health Care Consortium and $745 million for constructing mental health facilities.
“Year after year, the Texas Legislature has prioritized mental health funding, and the 2023 session will be no different,” he said in an email. “Lawmakers will work diligently to ensure communities large and small have the mental health resources they need.”
Local response
As the legislative session approaches, LaVar said the task force is working to complete its gap analysis in December with a recommendation of priority initiatives and longer-term needs. The analysis kicked off Sept. 20 with a meeting of about 100 stakeholders, LaVar said, and it will also include focus groups throughout the fall.
“What’s going to make the greatest impact right now?” LaVar said. “We’re going to produce for this county what we need right now and what we need to look at in the future.”
At the county level, Lt. Scott Spencer said the Montgomery County Sheriff’s Office received a $350,000 grant this year for two mental health professionals to assist with responses. The grant from the U.S. Department of Justice’s Office of Community-Oriented Policing Services was accepted by Commissioners Court on Oct. 25.
In addition, Burkhard said Mosaics of Mercy is working alongside Tri-County to assemble a public database of available mental health resources to help with the difficulty of finding a provider.
Dr. Deb Michel, clinical psychologist and national clinical director of virtual care with Pathlight Mood and Anxiety Center’s The Woodlands clinic, also cited additional stress caused by the pandemic as a major factor for the increased caseload mental health care providers are witnessing.
Michel and Bishai said both of their practices have been able to meet the increased demand for services through telehealth options so far.
“Our virtual eating disorder and mood and anxiety disorder programs, Eating Recovery At Home and Pathlight At Home, are able to meet the demand here in Houston and across the country by ensuring that our care providers are permanently licensed in several states so that access to treatment can be extended to a greater number of individuals,” Michel said in an email.
Roberson added it takes time for people to heal from a mass trauma incident, such as the coronavirus pandemic, and people are not there yet.
“People are still pretty raw, at least the people we see,” he said. “I believe that if we have another crisis of any significant sort, ... we would see an additional uptick of folks who are just not in a well state. It crosses all economic lines. ... People are just not doing that well.”
An economic crisis could precipitate further stresses, for example, he said. “If we were to see jobs start to shrink or hours to start to be cut at work, I think that could be the igniter of another mental health wave,” he said.
Vanessa Holt and Anna Lotz contributed to this report.