Experts say many technological investments have come about as a result of a need to refocus efforts for efficiency and safety and in light of increasing demand.
Houston Methodist The Woodlands Hospital and Memorial Hermann The Woodlands Medical Center are among the entities seeking to improve patient care and efficiency, having each completed $250 million hospital expansions in 2022 that included technological investments in new robotics, surgery equipment, and touchscreen and phone applications.
Nathan Way, director of acute care at Houston Methodist The Woodlands Hospital, said the changes, such as increased use of tablets for communication, were one of the only positive outcomes from the pandemic for the hospital.“Things we might have been pondering ... about, we pushed forward faster to get them here,” Way said during an April 13 media tour.
Justin Gnau, chief information officer for St. Luke’s Health, which has two hospitals in The Woodlands, said the hospitals had to adapt early in the pandemic by implementing telehealth. It also added artificial intelligence for the stroke management team and a virtual preceptor implemented in April to help the new nursing staff.
At Memorial Hermann The Woodlands Medical Center, President and CEO Justin Kendrick said the pandemic heightened the need for more accessible care and led to the use of virtual care visits.
“It was really accelerated to provide the experience for what people were needing at that time and will continue to need,” Kendrick said.
The pandemic has also changed the ways future health care workers are learning and incorporating technology into their curriculum. According to Lone Star College System and Sam Houston State University officials, nursing and osteopathic students have been learning through simulations using high-fidelity mannequins and electronic medical data.
Health care professionals said they hope the technological changes brought about by the pandemic will create greater access than previously seen.
“All of these technological advancements are interwoven,” Kendrick said. “Ultimately, ... we need to make certain our patients have access to the latest technology available to them.”
New technology
Kendrick said many of the technological changes at Memorial Hermann prioritize patient and employee needs as well as communication.
With its $250 million South Tower expansion—an eight-story project that added around 150 patient beds—Kendrick said some of the hospital’s new tools, such as cardiac care, are focused predominantly on patients age 50 and older. Information from the U.S. Census Bureau’s 2020 5-year Annual Community Survey estimates around 34.2% of The Woodlands population is age 50 or older with a median age around 40.
Four new catheterization laboratories added as part of the expansion use imaging equipment to visualize different parts of the heart and are among the most advanced in the country, he said. Memorial Hermann staff members state the tables for a cath lab run around $1.2 million each.
Kendrick said other investments have been made in telemetry monitoring for systems like respiratory rate and oxygen levels, which directly benefits care teams at the hospitals and provides safeguards within the catheterization labs to better protect employees.Investments have also been made in communications to keep patients’ families informed of their progress and to build out community spaces in the South Tower with audio and video equipment, he said.
Kendrick said his own family has made use of the hospital’s Everyday Well app during the pandemic for a virtual visit from a primary care physician when an incident came up with his father.
“Technology ... has been a way to enhance community,” he said. “If we have learned anything over the past two years, it is our reliance on technology and being able to have those types of capabilities, so we have been able to make sure all of our spaces are up to speed with the latest and greatest that is out there.”
Both Houston Methodist and Memorial Hermann have dedicated space and funding for advanced robotics in their expansions. Officials from both entities said robotics are used in surgeries, and dedicated spaces prevent the need for machines to be moved as often as they previously were.
At Houston Methodist’s Healing Tower, 106 new patient rooms have been equipped with tablets for a variety of purposes including video calls monitoring staff needs. Way said there have been additional initiatives to connect patients at the hospital, including adding Amazon Alexa devices into the new patient rooms.
“In the very [near] future, patients will be able to call their nurse using this device,” Way said. “They are going to be able to rapidly contact the team if they should ask for help in a concerning way. There is a huge future using this integrated technology.”
Way said to help patients who might not be as proficient with tablets and touch screens, Houston Methodist is developing an internal team for orientations with patients.
Aiding health care workers
Hospital executives have been looking for ways to use technology to help staff members, Kendrick said.
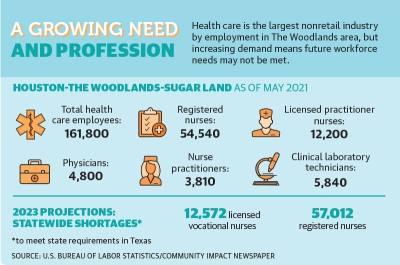
Information from an April report by the Texas Department of State Health Services states that by 2032, the supply of licensed vocational nurses is expected to grow by 13.8% to 79,179 across the state. However, the demand for LVNs is expected to increase by 45.5%, or 91,750, resulting in a deficit of available LVNs in the state by 2025.
The demand for registered nurses is also outpacing the supply. In 2018, there was a deficit of around 28,000 nurses in the state. By 2032, the deficit is anticipated to be around 57,000.
“The technology ... leverages their skillsets; it enhances their ability to provide care,” Kendrick said.
George Ludlow, senior vice president of marketing for Epion Health, which provides patient engagement products to health care providers nationally, said some of the main technologies his company uses include telehealth and digital intake options.
"Other technologies were well positioned to immediately address the unique conditions of the pandemic," Ludlow said in an email. "Scheduling software were available to manage the influx of patient volume for virus testing and care. Digital intake solutions were able to adapt quickly and add features to screen for [COVID-19] symptoms before in-person visits. Remote monitoring solutions were used to allow providers with a means to care for patients with chronic conditions, without added risk of virus exposure."
However, there are some areas in which telehealth is not applicable, said Dr. Sunil Raina, a physician and researcher for World Health Network, a global coalition of advisory teams.
“Technology advancements do not mean you are able to surmount this pandemic easily,” he said. “Surgical consultations may not be possible through telehealth, but diagnostics would see a huge benefit.”
Despite advancements in diagnostics and connecting with patients, Raina said there are some areas that will still need to rely on age-old techniques such as building trust between a doctor and patient.
Changes in education
Health care students have also adapted to using technological changes throughout the pandemic. At Lone Star College-Kingwood, LVN students have been learning on high-fidelity mannequins that can simulate human reactions due to a limited ability for clinical training, according to Nicole Townsend, faculty member with the LSCS nursing department.
“The pandemic has forced us to reinvent the wheel and lean more heavily on simulation,” Townsend said. “During the pandemic, pretty much everything was shut down. We were not able to go into the hospitals. ... It became more challenging for our nursing students, who are required by the Texas State Board of Nursing to get [a certain] number of clinical hours.”
Townsend noted that while the mannequins are not new technology, their latest iterations can be used to simulate a variety of scenarios that nursing students can experience while working, including various levels of bleeding, reacting to pain and giving birth. “It has been central to our nursing education, especially during the pandemic,” Townsend said.
Courtney West, associate dean of educational affairs at Sam Houston State University’s College of Osteopathic Medicine in Conroe, said students were able to still get hands-on experience, although in small groups throughout the pandemic.
West said students are also being trained with technologies such as mock electronic medical records, which are being used in area hospitals, and virtual training.“I know in our simulation centers, they have done interprofessional work where they have done a couple of scenarios,” West said. “Specifically, they interacted with an elementary school in Houston where they did a virtual simulation on a pediatric patient who was having an allergic reaction. They were able to do that through Zoom, and it was very well-received.”
West said she hopes the shifts in technology from the pandemic will increase access and opportunities for care with specialists.“I think that will enable us to grow the profession and provide more access to continuity of care moving forward,” West said. “That is the goal.”
Editor's note: The digital version of this story includes additional comments that were not included in the print version of the story due to space constraints.