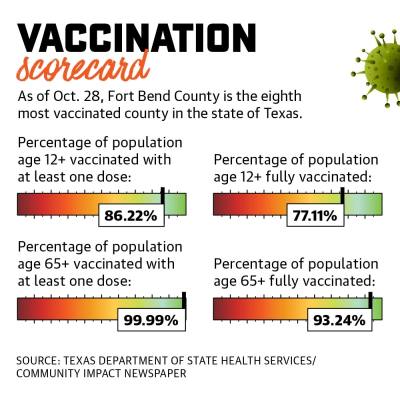
Additionally, 99.99% of residents age 65 and older—the most at-risk age group—have received one dose of the vaccine, and 93.24% are fully vaccinated. Fort Bend County Judge KP George attributed the county’s high vaccination rate to a number of factors, including its residents, who he said have responded to outreach efforts and initiatives.
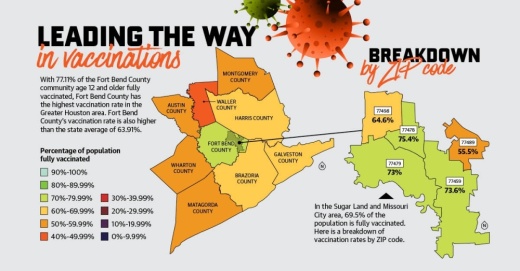
As of Oct. 28, Harris County lags behind, having vaccinated 67.44% of its population age 12 and older, while Montgomery County’s eligible population is 59.46% vaccinated.
“It’s very much a combined effort and a team effort where we were able to do a lot of things and guide people through the right channels,” George said. “The end results look like we are doing exceptionally well compared to many counties.”
Still, Fort Bend County is coming off a so-called “third wave” of new cases, driven largely by the delta variant’s transmission among mainly unvaccinated individuals, local health care officials said.
Fort Bend County Health & Human Services recorded the highest number of cases in one day since the pandemic began at 1,499 on Sept. 8.
“It’s extremely sad to have such a wonderful tool available for us [in the vaccine] and for whatever reason, people don’t take advantage of it,” said Kathryn Tart, dean of the University of Houston’s College of Nursing.
Combating coronavirus
Since Texas expanded eligibility for the vaccine in mid-May to everyone age 12 and older, FBCHHS has been working to make the vaccine as available as possible, officials said.
“Across the nation and here locally, vaccine uptake has decreased,” FBCHHS Director Dr. Jacquelyn Minter said in an email. “Although vaccinations are now more readily available, there are still those without easy access to commercial locations due to transportation, technology or working hours. Others are hesitant because of an unclear understanding regarding the vaccine’s safety, and others have heard incorrect or confusing information.”
Starting in July and continuing through September, FBCHHS reported an uptick in positive cases and hospitalizations as the delta variant spread in the community.
The seven-day average of new cases reported jumped from 20 cases in July to more than 350 in September. Meanwhile, the number of people hospitalized in Fort Bend County with COVID-19 rose from around 30 to more than 200 during that same time. As of Oct. 28, there are 2,488 active cases in the county.
Minter said of the cases reported to her department, 1.3% were confirmed to have occurred in people who were fully vaccinated. Fully vaccinated individuals are also less likely to be hospitalized or die because of the virus, Minter said.
Throughout the Houston Methodist Hospital system, 80% of patients hospitalized with COVID-19 are unvaccinated, said Dr. Nicholas Desai, chief medical information officer at Houston Methodist Sugar Land Hospital.
Desai said this most recent influx of COVID-19 patients has taken a toll on health care workers’ physical, emotional and mental health, and many feel the recent wave was preventable.
“It really hurts when you are seeing folks who are unvaccinated but yet then also have the ability to access those vaccines at such a readily available pace that it’s just emotionally draining,” Desai said.
Vaccine outreach
Despite the county’s relatively high vaccination rate, officials said vaccine outreach remains a top priority. Throughout spring and summer, Fort Bend County Commissioners Court approved spending federal aid to promote vaccine outreach, which has led to more people getting the shot, officials said.
In April, the county unveiled its Mobile Health Unit, which was funded through the Coronavirus Aid, Relief and Economic Security Act, and brings COVID-19 vaccines to underserved areas of the county. As of Oct. 20, the unit had provided about 9,000 vaccine doses to residents.
While the county was unable to provide a breakdown of funds spent on vaccination campaigns, George’s office said most of the efforts were funded using Federal Emergency Management Agency dollars, along with more than $8 million of CARES Act funding and more than $8 million from the American Rescue Plan Act.
The county has also used federal relief funding to provide aid to those affected by the pandemic, including through a child care voucher program, rent and mortgage assistance, employment incentives, and a small business assistance program.
“[FBCHHS] has transitioned from an all-hands-on-deck pandemic emergency response to an endemic response mode,” Minter said in an email.
Fulshear Mayor Aaron Groff said he applauds the county’s efforts to prioritize vaccine distribution and in making it readily available—but he said more funding for outreach efforts may not be needed.
“If people aren’t vaccinated today, it’s not because they don’t have access,” Groff said. “It’s because they’re making that choice not to, and so we don’t need to be continuing to spend dollars on initiatives to force something on people that are actively choosing not to participate.”
While the county is using funds for vaccination outreach and accessibility, it has stopped short of implementing incentives for people who get a shot—something Harris County has put money toward.
Harris County’s first incentive program awarded a $5,000 scholarship each week for 10 weeks to a student who received the vaccine at a county-run site beginning in June; its second program targeted the broader community by offering $100 for getting the shot. Both programs have since ended.
George said commissioners have considered incentives, but the high rate at which the county’s residents are getting vaccinated has not justified the need for them. Plus, he said he wants to be fair to people who have already gotten the shot.
However, some local business and community organizations have offered incentives.
In May, H-E-B hosted vaccine clinics at Constellation Field where vaccine recipients received a free Skeeters ticket. Meanwhile, the University of Houston, which has a campus in Sugar Land, offered students and staff $50 on their Cougar Card for getting vaccinated.
To reach unvaccinated groups, the county is bringing the Mobile Health Unit to schools, homeowners associations, businesses, places of worship and community organizations to make vaccines more accessible, Minter said.
“[These partnerships help] us to vaccinate even small numbers of people who might not otherwise get vaccinated,” Minter said.
Next steps in vaccination
Texas Gov. Greg Abbott issued an executive order banning all COVID-19 vaccine mandates Oct. 11.
Under the order, no entity can make the vaccine mandatory, including for customers or employees, punishable by a $1,000 maximum fine. Abbott cited the Biden administration’s Sept. 9 COVID-19 mandates for employers with more than 100 employees, calling the plans “federal overreach.”
Houston-area hospitals were some of the first private employers to mandate vaccines.
Desai said as health care workers, it is their responsibility to keep themselves, their families and their patients safe.
“We believe that is part of our Hippocratic oath to ensure we do no harm and to ensure that when patients put their lives in our hands that we follow the science and we are giving them the maximum protection from us,” Desai said.
However, others such as Groff said the decision to get a vaccine should be an individual’s choice.
“As a county, we have a high vaccination rate, both kids, adults and especially our senior adults,” Groff said. “And everybody’s got access.”