“Within a few days, [Katrina’s] health began to decline,’” Davis said during a May 21 panel discussion on Black maternal deaths in Harris County. “What happened is in delivery, she aspirated, and she became septic. ... At one point, we had my nephew in the [neonatal intensive care unit] and my sister in the [intensive care unit].”
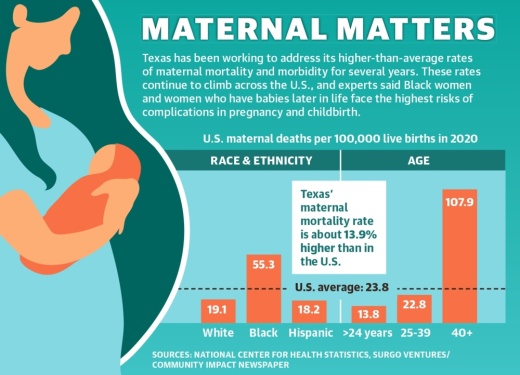
After four weeks in the hospital, Robinson died on May 26, 2007. According to experts, Robinson is just one of the many women who die each year due to pregnancy-related challenges, as barriers to health care have led to higher rates of maternal mortality in Texas than other parts of the U.S., with Black women and women older than age 35 facing the highest risks.
Dr. Manda Hall is the associate commissioner of community health improvement for the Texas Department of State Health Services and is one of 17 members of the Texas Maternal Mortality and Morbidity Review Committee.
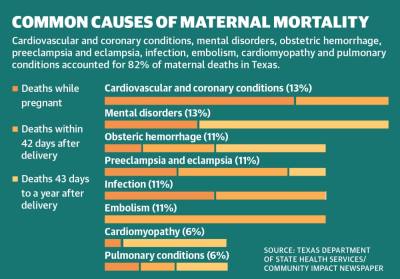
The committee’s September 2020 report stated cardiovascular and coronary conditions, mental disorders, obstetric hemorrhage, preeclampsia and eclampsia, infection, embolism, cardiomyopathy and pulmonary conditions accounted for 82% of maternal deaths in Texas.
“We know what we see as far as those leading causes of maternal death, and we also know that there are specific groups that bear the greatest burden of maternal mortality, meaning ... Black women,” Hall said.
The national maternal mortality rate was 23.8 per 100,000 births in 2020, an 18% year-over-year increase, which local health care providers said could partially be attributed to COVID-19. But Black women died at a rate of 55.3 per 100,000 births that year, according to the National Center for Health Statistics.
Hall said Texas’ maternal mortality rate consistently ranks higher than the U.S. average. The 2021 March of Dimes Report Card gave Texas a D and Harris County an F due to high rates of preterm births, infant deaths, inadequate prenatal care, social vulnerability factors and state policies.
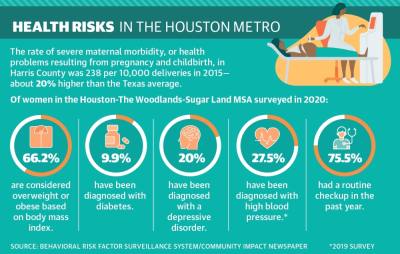
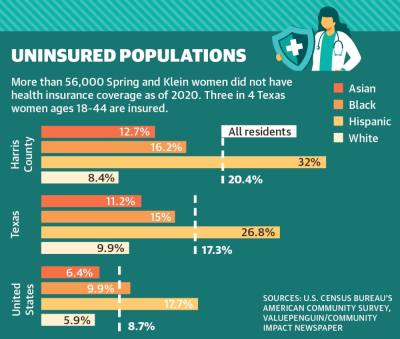
Dr. Ericka Brown, interim local health authority at Harris County Public Health, said the state’s elevated maternal mortality rates also correlate to its high rate of uninsured residents and other barriers to care.
“The Texas Medical Center sits in Harris County, and it’s a little bit astounding that unfortunately we still have some of the highest rates of Black maternal and infant mortality,” Brown said.
Identifying root causes
Researchers at ValuePenguin, an online data analysis tool, gave Texas the lowest score of all 50 states in a May study about access to and the quality of prenatal and maternal care.
Health insurance research analyst Robin Townsend said while Texas ranked in the middle of the country when it came to the quality of infant and maternity care, Texas had the lowest percentage of women ages 18-44 with insurance coverage at 73.6% and the lowest percentage of women who had access to a primary care provider at 57%.
“So not only are they not able to access a primary doctor, but they really don’t have a lot of options for paying for that,” she said.
According to the U.S. Census Bureau, 20.4% of Harris County residents were uninsured in 2020 compared to 17.3% statewide and 8.7% nationwide. Locally, 14.15% of Spring-area residents were uninsured.
“The way mortality is ranked for both mothers and infants, there are what we would consider provider causes and then there are what’s considered nonprovider causes,” Brown said. “For Black moms, the provider causes, unfortunately, are higher than they are for our white mom counterparts, and I think that speaks a lot to the inequity in the social systems and the support around our Black moms and our Black babies.”
ZIP code 77068 had among the highest rates of severe maternal morbidity between 2014-16, according to a study from The University of Texas Health Science Center at Tyler. About 21.9% of the 77068 population is Black, and 14.5% of 77068 residents were uninsured in 2020, per census data.
A single woman making less than $26,916 a year—a threshold nearly 30% of one-person households in the Houston-The Woodlands-Sugar Land metro area falls below—could qualify for Medicaid to cover prenatal visits, labor and delivery, and checkups up to two months after giving birth.
The Texas Legislature passed House Bill 133 in 2021, extending that coverage to six months after birth, but experts said women with comorbidities often need to be treated before conception and more than six months after delivering their babies. Brown said Black women tend to have higher rates of risk factors, such as hypertension, obesity and diabetes.
Dr. Rakhi Dimino, an OB-GYN at Houston Methodist Willowbrook Hospital, said more than half of births in Texas are covered by Medicaid, but many women do not receive prenatal care until later in pregnancy due to the lengthy process of obtaining coverage.
Texas has declined to expand its Medicaid program, which the Kaiser Family Foundation reported in 2020 would make 1.4 million additional nonelderly uninsured adults eligible for coverage.
Postponing pregnancy
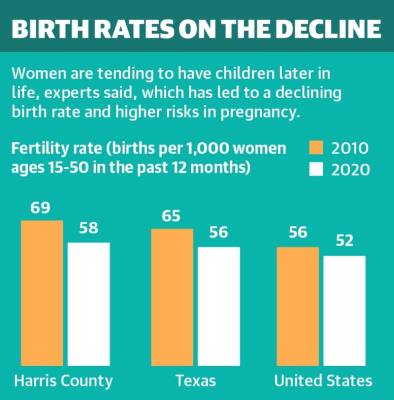
Dimino said when she started her career 17 years ago, many of her patients were having children in their 20s, and now she is seeing more women wait until their 30s and even 40s to have children.
“For many of them, it’s getting to a point in their career that they’ve invested in in order to support having a family,” she said. “And then once they are in that position, they are financially not having as many kids not just because of age, but the cost of raising a child is expensive.”
Harris County’s birth rate dropped from 81.5 births per 1,000 women in 2007 to 65 in 2019, according to the Centers for Disease Control and Prevention. Dimino said that trend has been exacerbated as women delayed pregnancy due to the pandemic.
The longer women wait to conceive, the more risks they can face in pregnancy and childbirth. The NCHS reported mothers age 40 and older faced a maternal mortality rate of 107.9 per 100,000 births in 2020. Women ages 25-39 died at a rate of 22.8 per 100,000 births.
“I think you have to respect the fact that there are higher risks as a woman gets older in terms of getting pregnant,” said Dr. June Marshall, an OB-GYN on staff with HCA Houston Healthcare Tomball.
Reducing the rates
One way local hospital systems, such as HCA Houston Healthcare, help care for mothers is by offering prenatal education. Media Relations Director Annette Garber said staff have also undergone bias training to help ensure Black women receive the same level of care as their peers.
“Pregnancy is serious. The rewards are great, but the complications and risk factors are as great,” Marshall said.
Statewide, nearly all hospitals that deliver babies participate in the TexasAIM to Reduce Maternal Mortality & Morbidity program, a DSHS initiative launched in 2018 to implement best practices in hospitals.
Locally, Houston Mayor Sylvester Turner; Harris County Precinct 1 Commissioner Rodney Ellis; and U.S. Rep. Sheila Jackson Lee, D-Houston, each presented proclamations declaring May 21 as Maternal Health Day.
Sima Ladjevardian, who serves as the regional director of Region VI for the U.S. Department of Health and Human Services, said the panel discussion was the first of what will become an annual event during which stakeholders will measure progress and continue to identify challenges.
“At HHS, we’re taking unprecedented actions to really make sure that these disparities are limited and we strengthen Black maternal health by expanding health coverage, implementing new policies and providing funding to ensure safer pregnancies and postpartum services,” she said.
Brown said Harris County Public Health plans to establish a program in late 2022 to target the county’s Black maternal mortality and morbidity rates. The initiative will help remove barriers to resources.