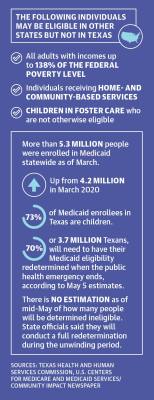
That requirement is still in place two years later, but health care advocates in Texas and Houston said they are worried about what could happen when it ends and millions of people have their safety nets put into jeopardy. The Urban Institute, a Washington, D.C.-based think tank, estimated as many as 1.3 million Texans could be deemed ineligible for Medicaid once the public health emergency ends.
Roughly 3.7 million of the 5.2 million Texans enrolled in Medicaid will have their eligibility redetermined once the emergency ends, according to the Texas Health and Human Services Commission.
Additionally, roughly 75.9% of Texas Medicaid enrollees are children, according to the HHSC.
Ezreal Garcia, public information officer for Community Health Network, which is a system of health clinics located in Brazoria, Galveston and Harris counties, said clinic operations have been impacted by COVID-19.
“We continue to work with our patients in getting them processed for recertification so that when that time does come, we can go ahead and process that information,” Garcia said.
The pandemic also shined a spotlight on a debate that has been ongoing in Texas since 2010: whether the state should expand Medicaid to cover more people. That debate will come up again when the state Legislature meets in January, and some local lawmakers said they are ready for change.
“We don’t have to go back to the way things were before the pandemic,” said state Rep. Ann Johnson, D-Houston.
State of Medicaid
The public health emergency was still in place as of May with an expiration date of July 15. However, the government also requires a 60-day notice before Congress can allow the emergency to expire. That notice was not given May 15, meaning the emergency is likely to be extended into October, per the Center on Budget and Policy Priorities, a nonpartisan research institute that analyzes federal and state budget policies.
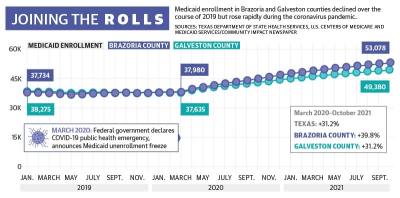
Since the emergency was declared, Medicaid enrollment has increased to its highest mark ever in Texas, hitting 5.3 million as of March, up from 4.2 million in March 2020, according to the HHSC.
In the Pearland and Friendswood area, the number of people enrolled hovered between 36,000-38,000 for both Brazoria and Galveston counties prior to the pandemic in 2018 and 2019. Since then, Galveston County rolls grew to 49,000 as of the most recent confirmed data from October 2021, while Brazoria County rolls grew to 53,000.
The HHSC’s preliminary data from February estimates around 55,364 Brazoria County residents and around 51,066 Galveston County residents are now enrolled in Medicaid.
When the public health emergency ends, a portion of Medicaid enrollees will have their coverage automatically renewed if they are deemed eligible. There will also be an unwinding period of up to 12 months during which states are to work with individuals who were not automatically re-enrolled to help them keep their coverage if they are still eligible, though a May 5 HHSC presentation on the end of continuous Medicaid coverage indicated that Texas plans to only use six months.
According to Farah Erzouki, senior policy analyst with the CBPP, for states to be successful, they will have to focus on two key areas: streamlining the application renewal process and communicating effectively with enrollees.“These steps will be key to make sure people can be reached, that they know what changes are coming and they know what they need to do to keep their coverage,” Erzouki said.
The CBPP recommends states increase capacity for renewals that are determined using electronic data matches, which will help avoid having to rely on enrollees to complete a renewal form or submit documentation, Erzouki said. Texas uses those kind of renewals in less than 25% of its processes, according to data from the Kaiser Family Foundation, a nonprofit focused on health care issues.
Additionally, Erzouki said it will be crucial for states to allow enrollees to renew their policies through a variety of methods, including online, by phone, by fax, by mail and in person. Texas is among the 33 states to allow renewals by all five methods, according to the KFF.
A looming crisis
There is no estimation from the HHSC at this time for how many people could be determined ineligible and unenrolled as part of that process, HHSC Press Officer Kelli Weldon said. Officials will get a better idea of that number after they conduct a full analysis during the unwinding period, she said.
The continued coverage requirement in the public health emergency has been quite beneficial to those on Medicaid, Garcia said.
Before the pandemic, individuals on Medicaid had to annually renew their policies, Garcia said, whereas those on private health insurance did not.
Garcia said he does have concerns about the timeline of the recertification process.
“We’re talking about millions of Texans that have not gone through the recertification process, and I am confident that the state will encounter challenges with the recertification process,” Garcia said. “That’s why we have done our due diligence to make sure that we’re educating our members and our patients.”
Children are most at risk of being unenrolled when the public health emergency ends, said Laura Dague, associate professor with the Texas A&M University Public Service and Administration Department who specializes in the economics of public health insurance.
“The vast majority—and that means, of course, the people who kind of stayed on [Medicaid] longer than expected—are low-income kids. I think we will see the most disenrollment in that group,” Dague said.
Debate over expansion
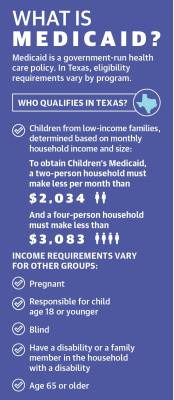
Certain population groups are required to be covered by Medicaid under federal law, including people who are below a certain income level and are also pregnant, are children, have a disability or are over age 65.
The health care policy is jointly funded by states and the federal government with the federal government paying 90% of the cost of health care for those insured by Medicaid and states paying 10%, according to the KFF.When the federal government signed the Affordable Care Act into law in 2010, each U.S. state was given the option to expand Medicaid coverage to nearly all adults with incomes up to 138% of the federal poverty level, an annual income of $17,774 for an individual in 2021, according to the KFF.
Texas is among 12 states in the country that have not expanded Medicaid. Of those 12 states, Texas also has set the highest bar for people to qualify based on income, only allowing people to enroll if they make less than $103 per month. Adults who do not have dependents or are not disabled do not qualify for Medicaid at all.
As a result, Texas has the highest rate of uninsured individuals of all states, according to the KFF. Nationally, about 10.9% of people are uninsured, compared to 20.9% in Texas. Researchers with Texas A&M University released a study into the economic effects of Medicaid expansion in 2019.
The study found expanding Medicaid would make almost 13,300 more people eligible in Brazoria and Galveston counties and result in almost 10,000 new enrollments. This would come at a cost of around $55.6 million each to the federal government and $6.1 million each to Texas.
Ahead of the next legislative session, which will kick off in January, several local representatives said Medicaid is top of mind. Those opposed to expansion said Texas would still be on the hook for about $500 million in program costs and questioned the effects it would have on improving health care outcomes in the state.
“Medicaid expansion is not fully funded by the federal government. Texas would have to pay for about 10% of the additional program costs, which would significantly reduce available funds for existing state programs and property tax relief. States who have expanded Medicaid have also seen increased costs over original estimates, so Texas may end up having to pay even more than presently estimated,” said state Rep. Cody Vasut, R-Angleton. “Medicaid expansion also does not necessarily equal expanded access to care. Many providers in Texas do not accept new Medicaid patients.”
State Rep. Ed Thompson, R-Pearland, whose district includes northern Brazoria County, declined to comment on the issue.Johnson said even if Medicaid is not expanded, there are things that can be done at the legislative level to improve the system.
“I think more and more legislators are realizing that even if we don’t expand Medicaid, there are improvements to the current system that can be made,” she said.