Lauren Cotton, the chief operating officer of the Greater Houston-based Neighbors Emergency Centers, said Neighbors ERs experienced an almost 30% decrease in volume since the beginning of the pandemic in America. Many patients are afraid by seeking help they will expose themselves to the coronavirus.
“It’s certainly concerning for health care providers because looking back at the reasons people come to the ER, most of those are completely non-COVID related,” Cotton said.
Dr. Carl Vartian, the chief medical officer for the HCA Houston Health Care Clear Lake and Mainland locations, said there has been a nationwide decrease in heart attack and stroke patients coming to hospitals or emergency rooms for treatment.
“People shouldn’t be afraid to come to the hospital for help,” Vartian said.
Cotton said she believes the coronavirus is going to change everything in terms of how the health care landscape operates.
“I don’t know of another time in modern history where the general population has been forced to stay home and really engage in a digital world, and I don’t think that’s going to be much different in medicine,” Cotton said.
Seeking medical help
Vartian, who is also an infectious disease doctor, said the number of people seeking treatment for noncoronavirus complaints went down noticeably during the first several weeks of the pandemic.
“We’ve seen a decline of women having mammograms, people getting cancer screenings, etcetera, and we need to reverse that because these people still need to be treated,” Vartian said.
Cotton said medical professionals across the board are seeing people staying home and not seeking care or waiting longer to get treatment until they reach a crisis point.
“Anecdotally, we’ve had patients tell us they thought we had better things to do right now, but not coming in right away when there’s a medical emergency makes your case more difficult in the long run,” Cotton said.
For medical events such as appendicitis, heart attacks, strokes and chronic illnesses that have been exacerbated, Cotton said the decrease in number was concerning.
According to data from the Houston Health Department, emergency calls for suspected heart attacks were down 50% from February to April.
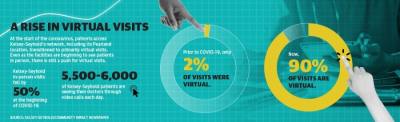
The situation has been slightly different for general practitioners and other nonemergency medical entities. Kelsey-Seybold clinics, which serve around 400,000 patients a year, have not experienced a significant decrease in volume.
Cherice Conly-Harvey is the managing physician for the Pearland Kelsey-Seybold clinic. She said the MyKelseyOnline service’s virtual visit option made the transition to not having in-person visits smoother.
“If I had to explain my experience, I would use the word intense,” Conly-Harvey said. “It was so sudden and so severe, what happened to us all, but I do feel like we did a good job early on taking care of both COVID-19 and non-COVID patients.”
According to Kelsey-Seybold COO Kenneth Janis, there was a short period of time during closures when in-person doctor visits fell by 50%. However, this does not mean the visits were not happening.
Prior to the pandemic, only 2% of visits were virtual. Now, 90% of Kelsey-Seybold patients are seeing their doctor through video calls, 5,500-6,000 of which are happening daily.
“I was really proud of our senior patients, who I know are sometimes intimidated by technology,” Conly-Harvey said. “They really stepped up and got on those video visits, and we were able to handle people’s blood pressure or diabetes diagnoses through these calls.”
The Kelsey-Seybold clinics resumed full normal operations May 18 after limiting face-to-face visits to only those absolutely necessary since March.
“We’re beginning to perform an increased number of elective procedures,” Janis said. “There is an ongoing process to not only increase visits, but to increase the availability of in-person visits.”
Preventive measures
Janis said Kelsey-Seybold approached the pandemic from three directions: keeping staff safe, keeping patients safe and maintaining a safe environment.
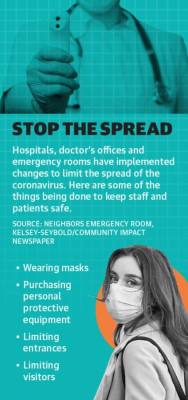
Maintaining a safe medical environment for patients and staff has been a priority across the county, and it has demanded facilities make changes to their workflow to accommodate new safety guidelines, Cotton said.
Kelsey-Seybold started screening employees and patients before coming into the clinic, following Centers for Disease Control and Prevention guidelines, and purchasing personal protective equipment.
In March, hospitals stopped performing elective surgeries, or procedures that can be scheduled in advance, and went through the process of minimizing the possibility of exposure by reducing visitors and visiting hours. Hospitals also limited entrances.
“We screen everyone coming into the building; doctors, CEOs, nurses, visitors, everyone gets screened,” Vartian said. “We also have universal masking, and every single person has been wearing masks for weeks throughout the hospital.”
Neighbors Emergency Centers also adapted its processes to limit exposure. Cotton said everyone wears a mask as soon as they enter the facility, and there has been a focus on getting patients to a room as quickly as possible so there is nobody waiting in the lobby.
“We are promoting that people call ahead if they need reassurances in terms of whether they should come in,” Cotton said. “We can also register them quickly and can get them right to a bed. That’s how we’ve been taking care of it as we’ve been setting up a telehealth platform.”
Long-term changes
HCA Houston Healthcare is beginning to reopen scheduling for elective procedures; the past months have required an absolute focus on those who could not wait for care, but Vartian said staff is slowly rolling back toward normal.
Vivian Ho, Rice University’s health economics chair, said telehealth is here to stay. Elderly and vulnerable patients will not be able to go out and resume normal daily life until a vaccine is available, which Ho said will lead to providers being pushed to figure out how to streamline electronic medical records.
Conly-Harvey said the Kelsey-Seybold virtual doctor appointments had been available for several years, but the pandemic emphasized how vital having that platform already established was.
“It was just a small portion of doctors that were doing it before, but I think there is a portion of people who have found they like the video visits and will always want it available,” Conly-Harvey said.
Janis also said having the infrastructure in place was important, and Kelsey-Seybold had been in the process of extending virtual services to more specialists before COVID-19 accelerated their plan.
Additionally, he said there was a chance wearing masks and checking temperatures when staff and patients enter a clinic may remain a policy in some iteration going forward.
“From an infection control standpoint, this will change how people think about the spread of diseases, especially with seeing how much trouble people are having with PPE, hand sanitizer, all these things that have always been accessible before,” Cotton said. “More and more ways to do things digitally from beginning to end will be developed, from follow-up to people accessing their own records.”
Cotton reiterated people can always call ahead to an emergency room.
“If you would have gone to the emergency room pre-COVID, you should go to the ER,” Cotton said. “We want to make sure we’re taking care of the communities we’re in.”
Hunter Marrow and Emma Whalen contributed to this report.