“Now that economy is opening, we should remember that [nursing homes] have the most vulnerable population, and it’s the population we need to keep safe,” said Rolando Amado, the executive director for Brightpointe at Rivershire, a skilled nursing facility in Conroe.
Statewide, there have been 3,325 confirmed COVID-19 cases among nursing home residents and 537 deaths as of May 21, according to the Texas Department of State Health Services. For assisted-living facilities, these numbers are 430 and 103, respectively.
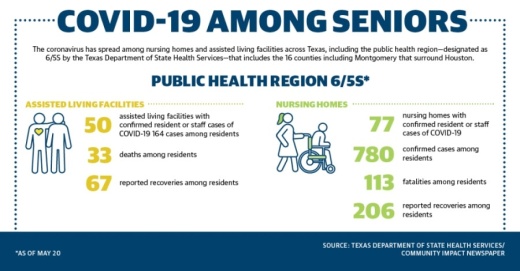
In the public health region that includes the 16 counties including Montgomery that surround Houston, there were 77 nursing homes with confirmed resident or staff cases of COVID-19; 780 confirmed cases among nursing homes residents; 113 fatalities among nursing home residents; and 206 reported recoveries among nursing home residents as of May 20.
In the same public health region, there were 50 assisted-living facilities with confirmed resident or staff cases of COVID-19, 164 cases and 33 deaths among assisted-living facility residents, and 67 reported recoveries among those facilities as of May 20.
And while the elderly account for only a small portion of Montgomery County’s cases, they represent a greater amount of deaths.
As of May 20, 48 of the county’s total 881 coronavirus cases are from individuals over the age of 80, according to the Montgomery County Public Health District. However, 13 of the county’s 21 coronavirus-related deaths are of individuals over the age of 80.
At least 21 of the county’s cases and at least two deaths stem from two nursing homes managed by HMG Healthcare: Park Manor of Conroe and Park Manor of The Woodlands, according to MCPHD. At least one other death has been reported from another unidentified long-term care facility in the county and at least three coronavirus-related deaths from The Conservatory at Alden Bridge, a luxury retirement community in The Woodlands.
On April 27, Brightpointe at Rivershire reported its first positive case, an infected patient who was returning from the hospital. Amado credited the facility’s strict procedures and practices as the reason the virus did not further spread.
“The day the test came back positive, the patient was sent back to the hospital and has remained there ever since,” Amado said. “Fortunately for us, nobody got infected.”
Testing troubles
On May 11, Gov. Greg Abbott released an order requiring 100% of nursing home residents and staff to be tested for the coronavirus. Community Impact Newspaper has reached out to the governor’s office for clarification on a timeline and funding source, but as of May 22, the office has not yet formalized details.
For local senior facilities, it is unclear on what the order exactly means for them.
“It is very loose. Right now we don’t know who’s covered in it,” Amado said.
Amodo said their facility was, in a way, fortunate to have already undergone testing. Following the positive case, the county hospital district tested all of the other residents May 6, and all results came back negative. The MCPHD covered the costs for these tests, he said.
Employees were also required to test themselves, but this was done through another lab the county did not pay for, and if an employee did not have insurance they had to pay out of pocket, he said.
Abbott’s order does not specify if counties will ultimately be responsible for administering tests. Although Montgomery County implemented a voucher program for coronavirus testing in mid-May, the county has struggled to provide enough free testing sites due to limited supplies and a backlog on orders.
To test every nursing home just once could cost Texas about $29 million and nationwide $440 million, according to a study by The American Health Care Association and National Center for Assisted Living. The cost is based on testing kits costing $150 and does not include assisted-living facilities or independent-living facilities.
On May 22, the U.S. Department of Health and Human Services announced $4.9 billion in funding to help skilled nursing facilities respond to the COVID-19 pandemic. According to a news release from the HHS, a portion of that money will go to expanding testing capabilities for nursing homes.