The best and brightest physicians were working on treatments while researchers searched for a vaccine.
Many patients were asymptomatic, but some suffered from a wide variety of symptoms: fever, sore throat, headache and fatigue.
As efforts to combat the disease grew, public fears grew because of the disease’s uncertain future and its devastating effects on vulnerable populations.
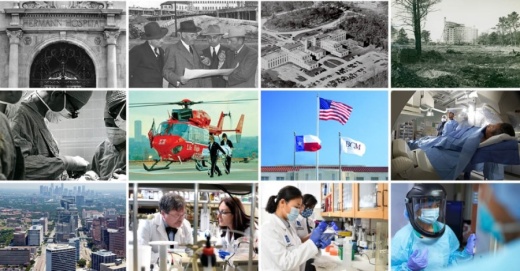
This is not 2020, and the disease is not COVID-19. This was the 1940s and 1950s, and it was the polio epidemic, the first public health crisis to test the budding Texas Medical Center, which was officially chartered 75 years ago as of Nov. 1.
The polio epidemic, in fact, continued to penetrate the United States in greater numbers than had ever before been seen, said Dr. Heather Wooten, an adjunct assistant professor for the Institute for the Medical Humanities, located at The University of Texas Medical Branch at Galveston.
Texas saw fewer than 1,000 polio cases in 1945, but by 1950, those numbers had increased to nearly 2,800 and then to almost 4,000 at its peak in 1952, according to medical statistics from 1945-58 kept by the nonprofit March of Dimes. In Harris County in 1952, there were 700 cases reported.
So when polio hit, it hit Texas, Houston and Harris County hard, Wooten said.
Ever since, the medical center has confronted challenges with pioneering medical practitioners and an eye to future collaboration and innovation.
Rising to the challenge
During the late 1940s to the early 1950s, a dangerous form of the disease, bulbar polio, which attacks nerve centers that control swallowing and talking and could lead to suffocation, had been on the rise, Wooten said.
“Most Americans thought polio was the most frightening thing, save for the atomic bomb, at the time because it affected children, the idea of America’s future,” said Wooten, the author of polio-focused book “The Polio Years in Texas: Battling a Terrifying Unknown.”Though the tank mechanical respirator, also known as the iron lung, had been developed years prior to provide breathing support, most hospitals did not have the capacity for multiple iron lungs, Wooten said.
Opening the Southwestern Poliomyelitis Respiratory Center—the first respiratory center in the country and what would be later known as the Texas Institute for Rehabilitation and Research—at Jefferson Davis Hospital was intended to remedy this with a focus on trained personnel and a room full of iron lungs, Wooten said.
Work on polio at the respiratory center and at the newly opened Texas Children’s Hospital, along with the Baylor College of Medicine being selected in 1961 as a site for trials of what would become the go-to polio vaccine, helped cement the TMC’s reputation.
“By doing that, it underscored the mounting prestige of the Texas Medical Center,” Wooten said.
Building and leaving legacies
The Southwestern Poliomyelitis Respiratory Center saw success in treating polio patients, but the director of the center, Dr. William Spencer, was a real driving force, Wooten said.
The TMC showed the world its prominence with the quality of the physicians it was employing, said Bryant Boutwell, longtime professor and former administrator for UTHealth.
“What happened was that Texas Medical Center became like a magnet for some of the greatest physicians in the country,” Boutwell said.
Recruiting world-renowned heart surgeon Michael DeBakey in 1947 was one such example that helped pave the way for the medical center’s future success.
“Michael DeBakey brought a lot of influence,” Boutwell said. “He was not only a great surgeon, but he had been decorated in World War II. He also had a lot of respect in Washington and could go there and walk the walls and could generate funding and support.”
In addition, DeBakey recruited another renowned surgeon, Dr. Denton Cooley, in 1951.
The duo collaborated on a number of innovations in surgery, including a new method of removing aortic aneurysms, the weak spots that can sometimes develop along artery walls.
But individually, alongside their teams, the two were pioneers.
DeBakey performed the first successful carotid endarterectomy—removing blockages in an artery—in 1953, and in 1958 he performed the first successful patch-graft angioplasty.
Cooley, who founded the Texas Heart Institute in 1962, went on to set multiple medical milestones, including one of the first heart transplants in the U.S. in 1967 and the world’s first total artificial heart implant in 1969.
Dr. Lee Clark was yet another leader, who put the medical center on the map for cancer care beginning in 1946 when he was named MD Anderson’s first full-time director and surgeon in chief. During Clark’s career, the cancer center opened in 1954, and he oversaw three major expansions to the complex during his 34-year tenure.Like Clark, DeBakey and Cooley stayed on at the medical center for decades, a common thread among early TMC leadership that was key to its continued success, Boutwell said.
“I think the early leaders set an example that you don’t plan for next year or the next after that, but you plan for the next decade or two,” Boutwell said.
The same applies to the TMC’s programmatic changes, according to Boutwell. The TMC leadership has and continues to take the approach of learning from the past and applying it to the future.
And with that has come a storied reputation that continues to build talent.
Dr. Maria Elena Bottazzi, co-director alongside her colleague Dr. Peter Hotez, and the team at Texas Children’s Hospital Center for Vaccine Development are one such example. The team, which worked on a COVID-19 vaccine that was licensed in August by India-based biopharmaceutical company Biological E. Limited for use in that country, came to Houston in 2011 after spending 10 years in Washington, D.C.
“The attraction for us to come to Houston was the fact that we were being recruited with this notion that we were coming to a very large ecosystem in health with the medical center,” Bottazzi said. “The recruitment was a joint venture amongst various institutions, including Texas Children’s and Baylor.”
Meeting needs
If there are some positives that have come out of the COVID-19 pandemic, it is how the TMC has increased collaboration among institutions more than ever before, said Dr. Marc Boom, the president and CEO of Houston Methodist Hospital System.
“What definitely continues to accelerate during COVID has really been more cross-institutional collaboration,” Boom said.
That includes taking a top-down approach to that collaboration, where seven days a week at 7 a.m., the CEOs of Texas Medical Center institutions touch base on needs and resources.
“And then there’s operational teams and supply chain teams and HR teams and ethics teams and others that have been functioning across the TMC,” Boom said.
This collaboration has taken the form of data sharing when the TMC releases daily updates on COVID-19 metrics, as well as equipment early on during the pandemic that was shared with institutions when needed.
“I think this experience has been a real-time dramatic episode where it further reinforced to us the value of collaboration,” Boom said.
And that collaboration extends to current and future efforts by the TMC as it seeks to continue to move health care forward for member institutions, said Dr. Bernard Harris, the vice chair of the medical center’s board of directors, which provides support for the TMC leadership team and approves all major decisions about the medical center.
To pursue that goal, the TMC has created institutions such as the Clinical Research Institute, which debuted in 2018.
“That is to help the institutions stay ahead of the latest and greatest technology that enables us to advance health care,” Harris said.
In addition, the institute has allowed a more seamless, unified interface for TMC institutions by allowing them to sign one set of documents that could, for example, allow them to have access to a new medical device or therapy.
The TMC is also increasing the work coming out of TMCx, an innovation center connecting entrepreneurs with TMC resources to create medical devices and digital health solutions. The TMC does this through its Venture Fund, which invests in innovative products from promising entrepreneurs, Harris said.
Investments include Alleviant Medical, which developed a minimally invasive device to treat congestive heart failure, and Corlnnova, which developed a soft robotic device that gently squeezes the heart in sync with the heartbeat to increase output.
These areas will continue to remain focuses as the TMC looks to expand its campus through TMC3, which is slated to open in 2022 and serve as a center between the TMC’s clinical and research campuses.
For Wooten, such innovation and presence in Houston paint the medical center in a central role.
“The Texas Medical Center is such an economic powerhouse,” Wooten said. “Not only the cancer research, but the biomedical portion of it is what keeps Houston what it is and evolved it from an oil town to this biomedical tech town.”