Ron Speidel was diagnosed with bladder cancer in 2013. By 2015, following chemotherapy and surgery, the cancer had spread to the bone.
With conventional treatment options exhausted, Speidel was told he had six months to live.
In April 2015, Speidel was approved for immunotherapy clinical trials at The University of Texas MD Anderson Cancer Center in the Texas Medical Center, where every 10 days over the next five months, he and 14 other cancer patients received experimental treatment. Immunotherapy consists of a series of drug infusions that take several hours each appointment.
The U.S. Food and Drug Administration approved the first immunotherapy drug in 2014 to treat melanoma. Although it was not easy, Speidel said he is still going strong seven years later—6 1/2 years longer than doctors gave him.
“It’s been a heck of a journey,” said Speidel, a retired Missouri police officer, in a phone interview with Community Impact Newspaper. “All the trials and tribulations I’ve had as a police officer, ... this has been a battle. This has been something I’ve never experienced in my life.”
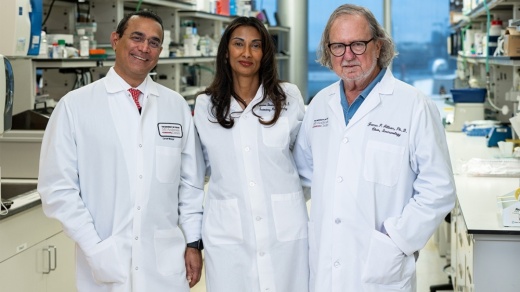
Key to researching the future of immunotherapy is the opening of the James P. Allison Insitute in Houston, run by MD Anderson and located in its medical center campus. The research hub is designed to further study new ways to treat cancer through the science of immunotherapy, said immunologist Dr. James Allison, for whom the institute is named.
“Immunotherapy has transformed cancer care over the past decade, but unfortunately, not all patients benefit equally. Our goal is to change that,” Allison said at the institute’s launch.
Making a difference
Between September 2020 and August 2021, MD Anderson Cancer Center conducted 1,600 clinical trials with 9,684 patients, according to its annual report.
Allison—who won the 2018 Nobel Prize in physiology or medicine in conjunction with Dr. Tasuku Honjo for work in immunotherapy as a means to treat cancer—leads the new institute with Dr. Padmanee Sharma and Dr. Raghu Kalluri.
The institute is expected to move to the TMC3 Collaborative Building upon its opening, with additional lab space to be added to their southern campus.
Immunotherapy emerged as a viable means of treating cancer over the last two decades, said Dr. Peter Pisters, president of MD Anderson Cancer Center.
“[Immunotherapy] is a broad term that really involves a series of strategies, based in science, that are designed to harness the immune system or to supercharge the immune system in different ways to fight the cancer,” he said.
The hospital made an initial investment of $15 million to the institute, and philanthropy will be an essential driver for progress moving forward, officials said. The institute plans to recruit 125 faculty and staff members over the next five years; that number is expected to double by 2032.
New kind of treatment

Around 66% of Texans diagnosed with cancer survive five years or more after diagnosis, according to a 2020 report by the Texas Cancer Registry.
Preemptive action is the most impactful way to fight cancer, Pisters said, noting one-third of all cancer cases are preventable. Diminishing tobacco smoking limits cases of lung cancer; reducing ultraviolet light exposure limits cases of melanoma; and proper weight control, diet and exercise fend off a host of diseases, including cancer, he said.
Historically, the three primary ways of treating cancer have been chemotherapy, radiation therapy and surgery, according to Pisters. Each method is used depending on the circumstances, and multiple can be used in conjunction with each other.
Traditional methods can have downsides that researchers said may be avoidable with the new treatment.
Chemotherapy is a drug treatment in which chemicals are introduced to kill fast-growing cells in the body. Because it is not targeted, chemotherapy can significantly affect the rest of the body, according to the Mayo Clinic.
“You can’t even hardly do anything,” said Speidel, who underwent chemotherapy for a year. “You’re so sick; you’re nauseated; you have blisters in your mouth. It’s terrible.”
Radiation therapy is the use of high-powered beams of energy to directly kill cancer.
“[Radiation] sometimes also targets normal tissues that are in the way, ... and this can create side effects that sometimes are self-limited and resolve after treatment but in some situations can be long standing and part of the survivorship experience,” Pisters said.
Immunotherapy is not without side effects, Speidel said. Checkpoint therapies have a 5%-10% chance of causing side effects, the most common being fatigue and inflammation, according to MD Anderson.
The types and severity of illness create a wide range in how much individuals are expected to pay toward care.
A year after treatment, Speidel’s thyroid shut down. However, Speidel said the downsides he has experienced with immunotherapy are nothing compared to the years of life he was given by undergoing experimental treatments all those years ago.
“All I do now is take a little pink pill in the morning for my hormones, and that’s it,” he said.