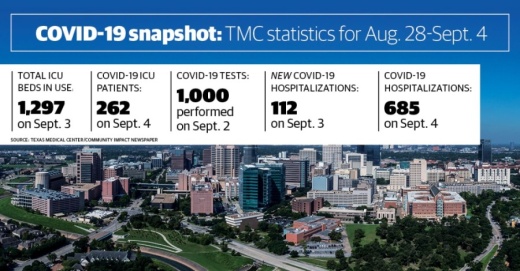
The medical center reported 685 COVID-19 patients in its hospitals, 81 fewer than compared to a week ago.
The total number of intensive care units in use saw a bump to 1,297, according to Sept. 3 data—up from 1,231 a week ago—though the number of patients hooked to those units with COVID-19 continued to decline, now at 262 from the 285 patients Texas Medical Center reported Aug. 28. This is below the 1,330-bed threshold that necessitates additional staffing and beds, as outlined in the medical center’s Phase 2 plan.
Data collected by the TMC spans hospitals in nine counties in the Greater Houston area, including Austin, Brazoria, Chambers, Fort Bend, Galveston, Harris, Liberty, Montgomeryand Waller counties.
Meanwhile, TMC hospitals reported that close to 1,000 COVID-19 tests were performed Sept. 2, with positivity rates down to 5%, down from its peak at 23% on July 9.
Baylor College of Medicine advises on preventing both COVID-19 and influenza
The Baylor College of Medicine medical hospital is reminding everyone that flu season is just around the corner, and that does not change because of the coronavirus pandemic, according to a Sept. 3 news release from Baylor.
“We take flu season very seriously every year, but this year it is especially important, since we’re now experiencing two respiratory infections that can have severe consequences simultaneously,” said Dr. Jill Weatherhead, the assistant professor of tropical medicine and infectious diseases at Baylor, in the release.
Weatherhead suggests getting a flu vaccine during September or early October prior to the onset of cases but said it is never too late to get a vaccine during the influenza season.
Differentiating between flu and COVID-19 symptoms can be difficult, Weatherhead acknowledged—both show fever, muscle aches, coughing, shortness of breath and fatigue—but a few isolated symptoms, such as loss of taste or smell, can be indicative. Still, Weatherhead recommended getting tested if unsure.
“There is significant overlap in clinical symptoms between influenza and COVID-19, making it difficult to differentiate the two diseases based on symptoms alone,” Weatherhead said. “Epidemiologic information, such as being in contact with someone who had the flu or COVID can help to aid in diagnostic accuracy.”