Hospitals prepared to convert new or unused beds for critical care and set up temporary medical tents that could be outfitted for medical treatment, according to Stephen Love, president and CEO of the Dallas-Fort Worth Hospital Council. Statewide, elective surgeries and procedures were put on hold in an effort to restrict social interaction and prevent hospital overcrowding, Love said.
But with more than 30,000 active cases and 2,000 fatalities as of June 17, coronavirus cases are on the rise in Texas, and the number of hospitalizations statewide has been increasing since early June, according to data from the Texas Department of State Health Services. In the region that includes Dallas-Fort Worth, the number of patients hospitalized with COVID-19 went up by nearly 16% to 765 patients between June 9 and 15.
For Medical City Alliance and a number of hospitals in the North Texas area, the effect of COVID-19 has been less than it could have been, said Matt Eiserloh, director of Communications for Medical City Alliance.
"It is really minimal, overall,” Eiserloh said.
Responding to a pandemic
A number of the Dallas-Fort Worth Hospital Council’s 90 members are part of larger systems, such as Medical City Healthcare and Baylor Scott & White Health.
Medical City hospitals have been offering free virtual screenings for the COVID-19 virus to determine a person’s risk level.
“It’s been a very interesting time to be in health care,” Medical City Alliance CEO Glenn Wallace said. “We’ve taken several steps to make sure we are able to respond appropriately to COVID-19.”
To consolidate resources, the Medical City Healthcare system has utilized its Dallas facility to conduct the majority of COVID-19 testing, Wallace said.
All COVID-19 patients at Medical City Alliance are quarantined in a dedicated unit, and their caregivers do not work with other patients to ensure it is safe to enter and work in other parts of the hospital, Wallace said. In addition, Medical City Alliance has enhanced visitor safety procedures by limiting hospital access, he said. All patients and visitors must enter through the emergency room entrance, everyone must wear a face mask or face covering and all patients and visitors are screened for COVID-19 through temperature checks and questionnaires.
“We’re educating patients on the precautions to ensure they’re safe and can come to the hospital if they need emergency care,” Wallace said.
Patient drop-off
One noticeable impact across the entire health care system has been a drop-off in patient numbers—first due to COVID-19 restrictions and then due to hesitance to seek care, along with confusion about guidelines from local and state officials, said Dr. Eric Huang, a dentist with Oasis Dental in Keller.
“We moved from seeing regular patients [in February] to only seeing emergency patients until May 4,” Huang said. “It was a problem when all you could see was, sometimes, only one or two patients per day.”
The decrease in patients has been the biggest challenge for Medical City Alliance as well, Wallace said. Visits to the emergency room decreased 27% overall, which has led to an increase in severe complications and death for all types of patients, he said.
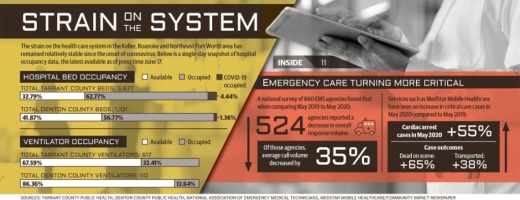
Across the Medical City system, there was a 70% overall drop in calls in April, Wallace said. The large drop-off in patient numbers coincided with a 34% overall decrease in calls to 911 nationwide, according to a National Association of Emergency Medical Technicians survey of 860 EMS agencies.
“We are quite concerned that locally and nationwide people are afraid, in some cases, to call 911,” Love said. “Hospitals and the emergency departments focus constantly on infection control. Rest assured, it is safe to seek emergency medical care with no fear of contracting COVID-19.”
“Make the call ... North Texas hospitals are here to serve you with safe medical diagnoses and treatment. There is no need to be scared, especially if your life depends on it.”
Cost of providing care
Though most COVID-19 restrictions have been lifted, medical and dental facilities have had to put stringent health guidelines in place.
At dental practices, for example, there is a concern about the spread of aerosol, a fine spray created during treatments. Guidelines require the use of N95 face masks and that lab gowns only be worn once per patient, Huang said.
“It’s about $30 per patient in PPE,” Huang said. “I have to hit every hardware store around the metroplex. But I have to take care of my patients. Some have been with me 20-plus years.”
After additional funds were spent to purchase PPE for employees in preparation for and during the ongoing fight against COVID-19, hospitals’ revenue streams continue to be impacted by executive orders in March and April that required medical facilities to postpone elective surgeries.
Those types of nonessential procedures are a significant part of a hospital’s bottom line, Love said.
“While I can’t comment directly on the financial operations of our hospitals, let me just tell you this. I know from experience: COVID-19 has been a severe financial hit to all hospitals,” Love said June 3.
Love’s comment followed an announcement in late May that Baylor Scott & White Health planned to lay off 1,200 employees, or 3% of the hospital’s total workforce. The decision was a result of a “drastic drop in visits,” the statement said.
Hospital revenue may have also been affected by a dramatic rise in people across the state losing their jobs during the pandemic, Love said. Because health insurance is tied to employment for many Texans, layoffs can lead to fewer people having the insurance they need to cover medical expenses.
“Fortunately, since we started performing surgeries again in late April and May, we have seen an increase in surgical volume,” Wallace said with regard to the financial situation at Medical City Alliance. “We are trying to keep our employees. If we can’t pay them due to decreased volume, we are paying them 70% of normal pay.”
Medical City Healthcare is also attempting to redeploy employees to sister facilities if they are qualified to work in a needed area, Wallace said. There are no COVID-19-related layoffs anticipated across the Medical City system, he said.
Despite the impact of COVID-19, progress continues on a two-story expansion to the Medical City Alliance tower, Wallace said.
“We will take a pause between now and the end of the year on completing actual patient rooms, but we will complete the tower because this is a very fast-growing area for patients in Alliance.”
Daniel Houston contributed to this report.