A March 22 executive order from Gov. Greg Abbott postponed all elective surgeries and non-emergency procedures. The order was part of an effort to conserve resources for those with COVID-19, he said.
Then came local orders that urged people to avoid going out except for essential activities. Local doctors said in-office visits dried up after that.
Bent Tree Family Physicians, which normally sees about 200 patients a day, had as few as five patients in its Frisco office at one point, founder Dr. Guy L. Culpepper said.
But as stay-at-home orders and restrictions on medical care have been lifted, people are slowly returning to their doctors.
have been lifted, people are slowly returning to their doctors.
“I believe that people need us,” Culpepper said. “People still get sinus infections and pneumonias, and they still get abscesses and rashes.”
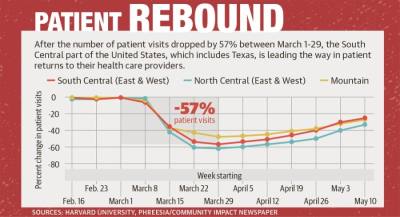
Nationwide, patient visits to health care providers declined by an estimated 57% in late March, according to national research from Harvard University and health care technology company Phreesia.
This decline has led Baylor Scott & White Health to announce May 26 that it will lay off 1,200 employees and furlough an undetermined number more across its health care system as it responds to a “drastic drop in visits.”
Bent Tree staff began rescheduling appointments in mid-March, Culpepper said, even before Frisco’s first stay-at-home order. That resulted in “very little revenue” coming in during the next six weeks, he said.
“I had to gather my 70 employees together, and I didn’t know what was going to happen in the next two weeks,” he said.
Culpepper decided to furlough his entire staff starting April 20.
He was not alone. A national survey of front-line primary care clinicians conducted from March to May by the not-for-profit Primary Care Collaborative survey found 42% of clinicians experienced layoffs or furloughed staff during the pandemic.
Dr. Bryan M. Lowery said his Frisco Concierge Medicine practice did not have to close, but business did slow down.
“Being a concierge practice, it’s a little bit different than your typical primary care practice,” Lowery said.
The practice does not rely on daily patient volume. Instead, patients pay a flat fee as part of the practice’s annual membership model. Lowery said because of that model, Frisco Concierge Medicine did not see the same revenue decline others did.
Dr. Scott Hastings said the patient load at his Family Medicine Plus practice in Frisco dropped by 90%.
“We were pretty heavily concerned for a couple of weeks, and then, we just started having more and more people coming in,” Hastings said.
While patient levels dropped, the demand for coronavirus testing remained strong.
The Texas Department of State Health Services reported more than 21,000 coronavirus tests in Collin County and over 19,000 in Denton County since testing began in March.
Bent Tree staff started doing coronavirus testing March 18, but protective gear was very limited, Culpepper said.
“I didn’t even know what an N95 mask was,” Culpepper said. “I’d never heard of that. We had a raincoat, goggles and a surgical mask. We just knew that people needed to find out if they’re sick.”
Culpepper estimated through mid-May, his practice had tested more than 350 people for COVID-19. About 60 patients tested positive, he said.
Lowery said he helped set up a drive-thru COVID-19 testing tent at Baylor Scott & White Medical Center—Frisco on March 17. That service, Lowery said, was testing 50 people a day at its peak and is still operating.
Hastings said he is encouraged to see patient numbers returning to normal. By mid-May, Hastings estimated Family Medicine Plus had rebounded three quarters of the way back to where it was before the coronavirus hit. He said he expects to return to previous levels by the end of June.
Lowery said business quickly rebounded at Frisco Concierge Medicine.
“It’s busier than normal because of all the COVID testing we’re doing and companies that are consulting me on how to get back to work,” Lowery said.
Culpepper sent an email in mid-April to Bent Tree’s approximately 30,000 Frisco patients about his decision to furlough staff. Patients started a GoFundMe page to raise money for the practice.
“It was kind of embarrassing because I’ve been a doctor for 32 years, and I’m the guy you’re supposed to turn to for help,” Culpepper said.
Thinking the effort might raise upward of $10,000 to help bring some of his staff back, Culpepper gave the page his support.
“It just went crazy, and all our patients started donating and brought it up to $90,000,” he said.
Culpepper said the second round of federal Paycheck Protection Program loans allowed him to bring back 90% of his staff, with plans to add back the rest.
“We will need to get to at least 80% of what we were doing before in order to be sustainable in the next couple of months,” Culpepper said.
Going forward, health care providers have made a number of changes to ensure patient safety and reduce the virus’s spread.
Lowery said he and many other doctors are worried about a possible second wave of COVID-19 in the fall.
The Primary Care Collaborative survey found 55% of responding clinicians fear they are unprepared for the next wave of the pandemic.
“If there’s another shutdown or people don’t feel comfortable going to the doctor and going to the store, that’s going to be a big deal,” Lowery said.