Could you describe your practice?
The nature of my practice is a little bit unique just given the patient population; the majority are uninsured, so access to specialty care is a challenge ... and then very high rates of comorbid mental health disorders, substance use disorders.
We prioritize very much social determinants of health, health-related social needs because my patients need housing and struggle with things like food insecurity and transportation. And we know in general those things are profoundly influential on someone’s health or lack thereof, probably more than any medicine I’m actually prescribing in clinic. And so we really pay close attention to that and help folks navigate housing and work closely with social workers, case managers.
How did COVID-19 affect your work?
Throughout the pandemic, one of the things I’m most proud of is we did ongoing surveillance testing of people who were living in the shelters, those on the streets surrounding and the staff. Over the course of the pandemic [we] did just over 1,000 COVID tests ... that helped prevent any further outbreaks in those settings and helped provide some advice and technical expertise to the shelters and other outreach and social service agencies around screening protocols and masking and COVID. And now we have pivoted, as most have, to vaccine-related work.
What are some challenges with connecting individuals experiencing homelessness to care?
Not to overgeneralize, but many people experiencing homelessness ... have a lot of inherent, and I would say not surprising, mistrust of the "system," including the health care system.
That I think stems from multiple reasons, some just sort of frank mistreatment and lack of compassion as they’ve navigated systems over time.
Health systems are intimidating. You need to sign up and be on time and get there and check in and get into a waiting room and you get thrust a whole clipboard of forms.
I just think all those things sort of stack up against them, and then when you add onto that mental health disorders and substance use disorders, which are historically stigmatized, that compounds it and then may even get in the way of your ability because of those illnesses, to navigate systems and appropriately advocate for yourself or address your needs.
It’s a learned skill to be able to take care of populations like this with unique needs and to have this level of compassion and empathy and be able to put yourself in someone else’s shoes who’s living in a world and navigating in a life that can be really hard to wrap your head around and inconceivable. And when you don’t have that understanding, it’s harder to show that empathy and compassion and easier to show judgment and disdain.
Historically it’s not a big part of medical school curriculums. I think it’s become better, and Dell Med is at the leading edge of that and around equity.
Was health care affected as public encampments became more prevalent in Austin?
If someone has a stable campsite and you know they're going to be under the same bridge and that’s where they identify as their home, temporarily, then that helps facilitate some access, I suppose.
That’s not me saying that I’m an advocate for dedicated campsites and unsheltered homelessness. ... There’s excellent data ... to show that unsheltered homelessness carries a tenfold higher risk of mortality, of dying, than the general population. Sheltered homelessness [is] about three times higher. So people who live in unsheltered homelessness have a much higher rate of morbidity and mortality; their average lifespan is in the low 50s, so from a health standpoint it’s not good for you.
Banning camping doesn’t do anything to get people into housing. ... Unless policies like that are married with pathways into housing, which necessarily require financial backing, then there’s just going to be those experiencing homelessness in different physical locations—and probably physical locations that aren’t as apparent.
That worries me that access becomes harder, and folks are going to be harder to find and more distant geographically from services which in many cities tend to be concentrated downtown or in certain areas, and we know that to be true in Austin.
What’s next for systems of health care for the homeless in Austin?
We certainly want to continue to do better, provide better care, improve the health. And that is done through making current services better, more patient centered, more trauma informed, of higher quality.
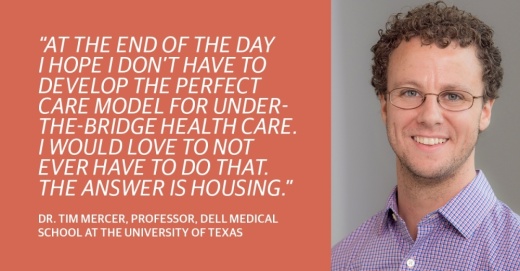
But also [by] innovating and expanding new models of care or scaling existing models that work. All that being said, at the end of the day I hope I don’t have to develop the perfect care model for under-the-bridge health care. I would love to not ever have to do that. The answer is housing.
And those are bigger policy and political and societal and financial questions that I didn’t go to medical school for. Housing I think is a human right, and shelter is a human right, and housing is directly correlated with health.
If we care about the people in our community being healthy and view this as a moral imperative, which I personally do ... then that should be our North Star end goal.