Suddenly, a nurse, wearing a face shield, smock and gloves rushed into the room.
“She told me to stop eating immediately,” said Tung, who had been diagnosed with COVID-19 a few days prior. “I was not getting enough oxygen.”
Over the course of the next few hours, a team of nurses and doctors attempted various methods of increasing oxygen flow—for one, asking Tung to lay on his left side and then to lay flat on his stomach, he said.
“Finally, the doctors said there’s nothing they could do,” he said. “They needed to intubate me.”
He was sedated, and a breathing tube was inserted into his windpipe while a machine pumped oxygen into his body.
Seven days later, Tung woke up.
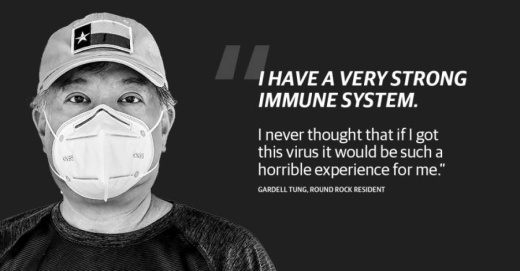
“I have a very strong immune system,” he said. “I never thought that if I got this virus it would be such a horrible experience for me.”
Tung, a native of New York, was visiting his mother in Queens in early March. He said he rode the subway into Manhattan a couple of times during his stay and suspects that may be how he caught the virus.
A veteran of the United States military, Tung described himself as the kind of person who rarely gets sick.
“I thought that if I were to catch this virus, I would be asymptomatic or just have mild flu symptoms,” he said. “I even made fun of the virus on Facebook.”
After returning to Round Rock on March 18, Tung said, he began to feel feverish. He called Veterans Affairs, a medical service and insurance provider for former U.S. military service members. They asked him a series of questions and said there was a good chance he had COVID-19 based on his recent travel history and symptoms.
Tung said the VA recommended self-isolation. Over the course of the next five days spent at home, he described his symptoms as similar to “a bout of bronchitis.” He coughed up phlegm that at first was green, then brown. And then, he coughed up blood.
“That worried me,” Tung said. “I felt that I needed to go to the ER.”
He arrived at the medical center around 3 p.m. March 23. He was given a mask and triaged “within minutes,” he said.
“If I were still in New York, I would have had to wait five or six hours,” Tung said. “They probably would have sent me home. I probably would have died there.”
Tung said he remembers his temperature registering 104 degrees. He said medical staff took a chest X-ray and then a CT scan, which revealed pneumonia in both of his lungs.
“By midnight, I was in intensive care,” Tung said.
A swab test was sent off for evaluation and came back the next day with a positive result for COVID-19.
“At Baylor Scott & White Health, there is nothing more important to us than the well-being of our patients and staff and the broader health of our communities,” spokesperson Christina Millweard said in an email to Community Impact Newspaper. “New measures and protections are in place across our hospitals, surgery centers and clinics, in accordance with CDC guidance and recommendations by our clinical experts.”
Since March, more than 90% of the hospital care provided at Baylor Scott & White has been unrelated to COVID-19, Millweard said. Baylor Scott & White declined to give specific numbers of COVID-19 tests administered and patients treated at this time.
“During this unprecedented time, our teams are faithfully serving those who need us most, and we are proud to be part of a community with a strong desire to make a difference,” Millweard said in the email.
Members of the medical team that cared for Tung were covered head to toe in personal protective equipment, he said. Though he said he was kept in an isolation ward within the intensive care unit, he said he felt anything but alone.
“The nurses and really the whole staff were very comforting. I can’t believe how well they cared for me,” he said. “They were literally putting their health at risk to take care of me, and that’s why I have such a high regard for them.”
Upon waking from a weeklong sedation, Tung described feeling weak from lying in bed without any physical activity.
“Just the act of walking and maintaining my balance was very tough after being in bed for so long,” he said. “Even sitting up in bed made me dizzy and nauseous.”
Several days later, he was tested twice within 48 hours for COVID. Once both tests came back negative, he was discharged April 10.
“I’m back to normal,” he said, approximately one month after being discharged. “Well, the new normal. Everybody is dealing with a new normal right now, I suppose. Life is going to be a bit different from now on for all of us.”
His mother, who is in her late 80s, continues to isolate at home but has not shown any symptoms of the virus, Tung said.
“I can honestly say that in New York City, many of my friends have already gotten this. A majority of them were able to nurse themselves back to health from home,” he said. “They did not require hospitalization. But I also know friends that have died from it.”
He added, finally: “This virus is real. Take it seriously, take precautions, but don’t panic.”