According to the Centers for Disease Control and Prevention, MIS-C is a condition in which different body parts can become inflamed, including the heart, lungs, kidneys, brain, skin, eyes or gastrointestinal organs. Symptoms of MIS-C vary and can include fever, abdominal pain, vomiting, diarrhea, neck pain, rash, bloodshot eyes or extreme fatigue.
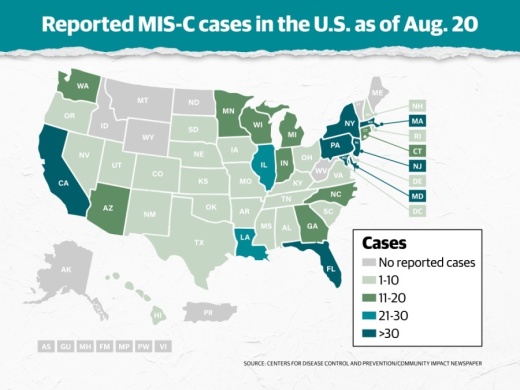
As of Aug. 20, the CDC reported 695 confirmed cases of MIS-C across 42 states, New York City and Washington D.C., 11 of which have resulted in death. Of those confirmed cases, 99% tested positive for SARS CoV-2—the virus that causes COVID-19—and the remaining 1% had been exposed to someone with COVID-19.
According to the CDC, most children who develop MIS-C develop it two to four weeks after being infected with SARS-CoV-2. All confirmed cases have occurred in children, from as young as less than 1 year old to 20 years old, with the average case being 8 years old. Additionally, 70% of confirmed cases have occurred in children who are Hispanic, Latino or non-Hispanic Black, and 55% of confirmed cases have been male.
Dr. Sandy Hong is a clinical professor at the University of Iowa Stead Family Children's Hospital, and she has been in the practice for 19 years. She also serves as the chair for the American Academy of Pediatrics Section of Rheumatology. Hong recently spoke with Community Impact Newspaper to share her thoughts on MIS-C, the questions that still remain and what parents should know about the condition as their children return to school.
This interview has been edited for length and clarity.
Can you briefly explain what MIS-C is as well as the associated symptoms are?
Current thinking is that MIS-C is an immune response associated with COVID-19 infection that causes systemic inflammation. This inflammation can affect many organs, including the intestines, skin and the cardiovascular system/heart. Patients are presenting with fever, rash, abdominal pain/vomiting and evidence of systemic inflammation on blood work. They also are presenting with evidence of cardiac abnormalities and some patients have developed inflammation in the heart vessels. Patients have presented with cardiovascular collapse; other [patients], with inflammation and rash and coronary vessel dilation similar to that seen in Kawasaki disease. Kawasaki disease is also thought to be due to peri-/post-infectious immune stimulation and dysregulation. Suspicion for MIS-C rises if a patient has Kawasaki-like disease or sudden cardiovascular compromise and has had recent exposure or infection with COVID-19 and other sources of the fever and symptoms have been evaluated. MIS-C is rare and is not necessarily the first thing parents and doctors should be worried about when children have fever.
Do physicians know yet how MIS-C is contracted? If so, how? Are some children more prone than others?
We don’t have enough evidence to say if some children are more prone than others to developing MIS-C. We think this is a peri-infectious phenomenon associated with COVID-19 infection. So, if you don’t get COVID-19, you are unlikely to get MIS-C.
How is MIS-C treated?
There is no evidence about how to best treat MIS-C. Treatments have been tailored to each patient. We know many patients have received fluids, blood pressure support, intravenous immunoglobulin [and] steroids, and some have received biologic agents, such as Anakinra or Actemra. Some patients have received aspirin or blood thinners to prevent clotting. Many patients with MIS-C have been noted to have increased risk of clotting. The intravenous immunoglobulin, steroids and biologic agents all work to calm the immune system.
How common or rare is MIS-C?
MIS-C is rare. As of Aug. 20, there have been 694 confirmed cases of MIS-C diagnosed in the U.S. According to the American Academy of Pediatrics—who is doing a wonderful job trying to count children as no one source is doing this—442,785 children have been tested as infected with COVID-19.
As many parents and guardians are currently making the choice between remote and in-person learning, do you think the possibility of MIS-C is something that should be taken into consideration? Why or why not?
MIS-C is rare. I think that parents should focus on the effect of COVID-19 on the health of vulnerable family members overall.
What are some of the unknowns still surrounding MIS-C? What studies are ongoing to better understand these unknowns?
We are not sure of the best way to treat it. There are collaborations that are tracking patient cases to figure out which medications are best. We are not sure about the long-term complications to the heart for those patients who have had evidence of heart involvement/inflammation of the heart vessels.
If a parent suspects their child has MIS-C, what protocol should they follow?
If a parent has concerns about MIS-C they should talk to their pediatrician. Pediatricians are aware of MIS-C, and the American Academy of Pediatrics has guidelines for evaluation of MIS-C. Because MIS-C is a multi-organ disorder, a patient suspected of having MIS-C will likely have a team of people to take care of them, including rheumatologist, cardiologist, infectious disease specialist, hematologist and sometimes intensivist.