The need for more telehealth systems in the area has long been a topic of discussion among local health experts. Harris County Public Health released the “Harris Cares: A 2020 Vision of Health in Harris County” in November. The report recommended HCPH invest in more versatile alternatives to standard hospitals and clinics, including mobile health vehicles and telehealth.
Dr. Sherri Onyiego, interim director of nutrition and chronic disease prevention at HCPH, said via email transportation barriers and health insurance can deter people from seeking health care in traditional settings, pushing the need for more mobile and telehealth services.
“It is important to offer alternatives to traditional ‘brick and mortar health care’ given that health truly happens outside the four walls of the traditional health care system,” she said.
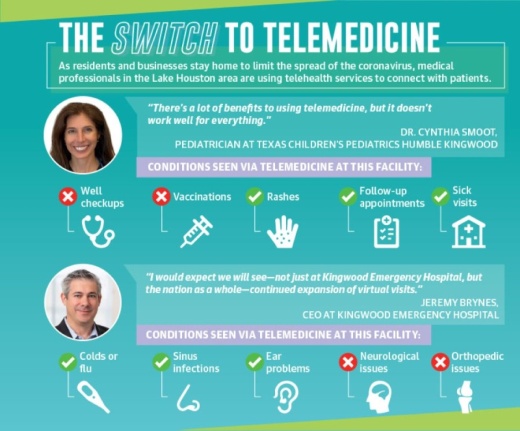
Some Lake Houston-area facilities and hospitals have launched telehealth services during the outbreak to meet the increasing needs of the community.
Meanwhile, other Lake Houston-area medical practices have been offering some form of virtual assistance for years, such as UTMB Health, which cares for 80% of the state prison population via telehealth, or My Eyelab in New Caney, which relies on telehealth for its business model.
Stepping up to serve
The need for these services became more apparent to Kingwood Emergency Hospital CEO Jeremy Brynes when the coronavirus pandemic hit the region. As more residents stayed home the hospital was inundated with calls, Brynes said. In mid-March, the hospital launched telehealth services.
“We wanted to make sure people had access to get the right information ... [and] that we gave them the opportunity to ask from the safety of their homes questions of a physician,” he said.
Telehealth services are also beneficial for patients looking for affordable health care options. A telehealth visit at the hospital will cost a patient a flat rate of $30—what many insured patients might have as a co-pay, Brynes said.
“We wanted to give people a way of saying, ‘You know what, [for] $30 I can speak to a doctor, get a prescription if I need it and get advice on whether I should be concerned,’” he said.
Brynes said the hospital may continue to offer telehealth services.
“I think people that gain more experience with virtual visits will find it’s a great alterative to a physical environment to get care,” he said.
Meanwhile, Dr. Cynthia Smoot, a pediatrician at Texas Children’s Pediatrics Humble Kingwood who has worked at Texas Children’s Pediatrics for 17 years, also began offering telemedicine in March.
In the past, Smoot said she would accept photos from patients’ families if needed to help in diagnosing a medical issue without an in-person visit, but the coronavirus pushed Texas Children’s Pediatrics to launch telehealth services.
Smoot said telemedicine still cannot replace specific types of pediatric appointments, such as checkups. However, about 25% of her patients switched to telehealth services during the pandemic, she said.
“I think for follow-ups, for certain rashes, for just questions, there’s a lot of benefits to using telemedicine,” she said. “But it doesn’t work well for everything.”
Foot in the door
For some medical offices and facilities, telehealth services were already a major part of practice. Ryan Galvez, managing partner of My Eyelab in New Caney, said the optometry franchise specializes in offering telemedicine and selling eyeglasses from its brick-and-mortar office.
My Eyelab offers patients the ability to get an initial assessment with a patient coordinator, then meet with an optometrist remotely. Benefits of the semi-remote appointment include quicker appointments and access to doctors who speak various languages, Galvez said.
“This method can take care of just about 91% of everybody that comes in through our doors,” he said.
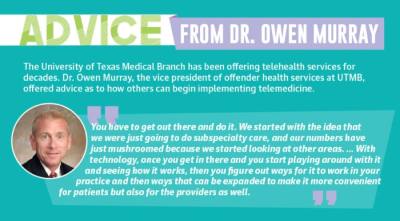
Additionally, the University of Texas Medical Branch has been offering telehealth services for decades, with UTMB Health physicians providing virtual medical, dental and mental health services for adult and juvenile inmates across Texas’ prison system. Dr. Owen Murray, vice president of offender health services at UTMB, said the system cares for about 80% of the state’s prison populations.
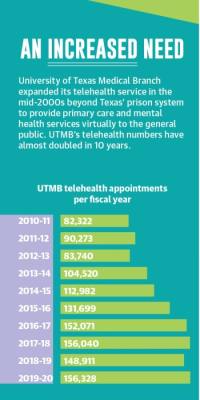
UTMB Health expanded its telehealth service in the mid-2000s beyond Texas’ prison system to provide primary care and mental health services virtually to the public. In the last 10 years, UTMB’s telehealth numbers have almost doubled from 82,322 appointments in fiscal year 2010-11 to 156,328 appointments in FY 2019-20.
While UTMB has had great success with telemedicine, Murray said there are some specialties where practicing telemedicine will not be as effective as in-person appointments.
“Being able to do both subspecialty care, mental health care as well as primary care, telemedicine is an excellent vehicle,” he said.